Abstract
We report a case of Osborn waves occurring in a 55-year-old normothermic male patient with spontaneous pneumothorax that resolved with the resolution of the pneumothorax. The patient was presented with a 2 week history of shortness of breath, pleuritic chest pain, and cough. He was found to have a left sided pneumothorax that persisted even after chest tube placement. The Electrocardiography (EKG) showed Osborn waves. He had a normal temperature, normal electrolytes, and a normal echocardiogram. Pneumothorax resolved after pleurodesis and pleurectomy. Post-operative EKG showed complete resolution of Osborn waves.
Keywords
Pneumothorax, Hypothermia, Electrocardiography, Chest tubes, Video-assisted thoracic surgery
Learning Objective
To report a case of Osborn waves occurring in a normothermic patient with spontaneous pneumothorax that resolved with the resolution of the pneumothorax.
Introduction
Osborn waves, also known as J waves or the camel-hump sign, are a characteristic electrocardiogram (ECG) finding associated with hypothermia. They are typically seen as a positive deflection at the J point of the ECG waveform, creating a characteristic hump-like appearance. These waves are believed to result from altered ion channel function in cardiac cells due to the effects of hypothermia on the myocardium. The exact mechanism is not fully understood, but it is thought to involve changes in transmembrane potassium and calcium currents, leading to delayed repolarization of the ventricles [1].
Osborn waves are best seen in the inferior and lateral precordial leads. They have been widely reported in the literature as hypothermic waves because they become more evident as body temperature decreases (<90°F), and they resolve gradually with rewarming [2]. Other associations include hypercalcemia, cardiopulmonary arrest from over-sedation, brain injury, subarachnoid hemorrhage, ventricular fibrillation, and vasospastic angina [3]. We present this case to underscore that while existing literature does not establish a link between Osborn waves and pneumothorax, our findings demonstrate the presence of Osborn waves in the context of pneumothorax. This report aims to contribute to the understanding of this potential association.
Case Presentation
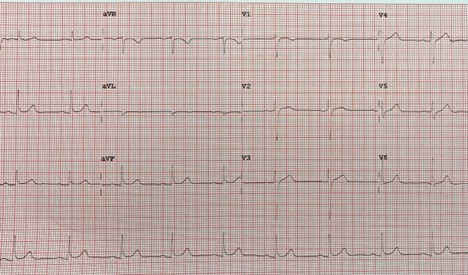
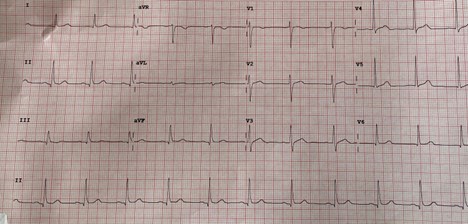
A 55-year-old man with past medical history of spontaneous pneumothorax 8 years ago presented to the emergency room (ER) with a 2 week history of shortness of breath (SOB), pleuritic chest pain, and cough. His symptoms worsened in the last two days, which prompted the emergency room visit. He denied any recent history of trauma, travel, cigarette smoking, or alcohol use. Vitals on presentation were within normal limits. A chest X-ray performed in the ER showed a large left upper lobe pneumothorax with minimal rightward mediastinal shift. Despite the placement of a left chest tube, residual pneumothorax persisted. Thoracic surgery was consulted on pleurodesis via left sided video assisted thoracoscopic surgery (VATS). As part of the pre-operative evaluation, an EKG was performed that revealed Osborn waves (Figure 1). At the time of the EKG, the patient was normothermic (98.1°F) and had normal electrolytes (especially calcium, sodium, potassium, and magnesium). His echocardiogram showed no structural or wall-motion abnormalities. The patient subsequently underwent VATS with chemical pleurodesis and parietal pleurectomy. His post-operative EKG showed the resolution of the Osborn waves (Figure 2).
Figure 1. EKG showing Osborn waves in inferior leads.
Figure 2. Post-surgical EKG showing resolution of Osborn waves.
Discussion
Osborn waves occur as a consequence of a prominent cardiac transient outward potential current (I to )-mediated action potential notch in the epicardium, giving rise to a transmural voltage gradient [4]. Normally, it is the transient inward potassium current that gets activated during phase 1 of the cardiac myocyte action potential [5]. Some case reports have cited the presence of Osborn waves in normothermic patients and in patients with severe hypercalcemia [6]. To our knowledge, only one other case of Osborn waves in a normothermic patient has been attributed to pneumothorax [7]. In that case report, Osborn waves were seen in the inferior and precordial leads in a 55-year-old male with a hydropneumothorax and myocardial ischemia. Unfortunately, the patient suffered a cardiac arrest before further investigations could be performed, and the authors remained unsure if the Osborn waves should be attributed to the hydropneumothorax or myocardial ischemia. Our case convincingly establishes an association between Osborn waves and pneumothorax based on the EKG appearance, the elimination of other potential causes for Osborn waves, and the resolution of the Osborn waves after the resolution of the pneumothorax. Our patient’s EKG showed the classic Osborn waves in leads II, III, and avF. His multiple temperature measurements remained in the normal range. He had a completely normal panel of electrolytes. His echocardiogram showed no structural abnormalities or wall motion abnormalities. His serial cardiac troponins were negative. The resolution of Osborn waves after the complete resolution of pneumothorax has never been reported in the literature.
Conclusion
This case highlights pneumothorax as a possible reversible cause of Osborn waves in someone with normal body temperature, normal electrolytes, and normal cardiac anatomy. Osborn waves seen with pneumothorax are completely reversible after the complete resolution of pneumothorax, as seen in this case. More systematic studies can be performed to establish frequency of this association, as it can implicate Osborn waves as a potential diagnostic tool for spontaneous pneumothorax.
Conflict of Interest
This manuscript is original research, has not been previously published, and has not been submitted for publication elsewhere while under consideration. The authors declare no conflict of interest in this manuscript.
Authorship Statement
AAF and SL designed the study. All authors performed the study, contributed to data extraction, reviewed the literature, analyzed the data, and wrote the paper.
Financial Disclosure
This paper did not receive any financial support.
References
2. Alhaddad IA, Khalil M, Brown Jr EJ. Osborn waves of hypothermia. Circulation. 2000;101(25):e233-e44.
3. Antzelevitch C. J wave syndromes: molecular and cellular mechanisms. J Electrocardiol. 2013 Nov-Dec;46(6):510-8
4. Grant AO. Cardiac ion channels. Circ Arrhythm Electrophysiol. 2009 Apr;2(2):185-94.
5. Burali A, Porciello PI. Onda di Osborn in pazienti normotermici? [Osborn wave in normothermic patients?]. G Ital Cardiol. 1991 Sep;21(9):1005-9.
6. Otero J, Lenihan DJ. The "normothermic" Osborn wave induced by severe hypercalcemia. Tex Heart Inst J. 2000;27(3):316-7.
7. Chauhan V, Brahma RS. Osborn waves in normothermic patient with hydropneumothorax and myocardial ischemia. Int J Crit Illn Inj Sci. 2015 Oct-Dec;5(4):268-70.