Abstract
Introduction: After rapid implementation of telehealth delivery of rehabilitation services at the outset of the COVID-19 pandemic, there was a lack of information on rehabilitation providers’ perceptions of the usability of telehealth in rehabilitation and their satisfaction with telehealth.
Methods: Rehabilitation providers (n=68) at an academic medical center and county hospital who delivered care via telehealth from March to August 2020 were assessed via a survey study (54% response rate) which gathered information on types of encounters, provider satisfaction, challenges faced, and usability as assessed by the Telehealth Usability Questionnaire (TUQ; subscale scores ranging from 1-7).
Results: Rehabilitation providers reported telehealth was useful (TUQ Usefulness subscale mean 6.27, SD=0.76), easy to use (TUQ Ease of Use subscale mean 5.72, SD=1.05), and effective (TUQ Effectiveness subscale mean 5.33, SD=1.03). They were overall very satisfied with telehealth (TUQ Satisfaction subscale mean 5.81, SD=1.03). Just under half (41.2%) experienced issues, with technical problems (e.g., connection issues) and limitations of technology (e.g., unable to perform physical examinations) as the most common. Traumatic injuries, stroke, wounds, pain, and urinary/bowel dysfunction were the most challenging conditions to address using telehealth.
Discussion: Despite this being the first time that almost all participants had used telehealth in clinical practice as a direct result of shutdown of in-person services in response to the pandemic, rehabilitation providers were highly satisfied with using telehealth, finding it to be useful, easy to use, and effective. The rapid and effective implementation and positive provider experience indicate that telerehabilitation could be maintained to improve access to clinical services and efficiency in service delivery.
Introduction
Telehealth has been around since the 1960s as a healthcare delivery modality, though it did not gain widespread acceptance as a viable and reliable clinical tool until the late 1990s, when digital imaging and high speed, high bandwidth telecommunications technology became widely available [1]. Historical boundaries to its acceptance and application have also gone beyond just the state of technology and have included such varied issues as state licensure regulations and reimbursement restrictions, as well as potential ethical conflicts for healthcare providers and patients [2,3]. Nonetheless, over the past three decades, and in particular the last decade, interest in telehealth application and integration into healthcare delivery models has continued to grow due to its promise and improved access to telecommunications platforms.
The adaptation and application of telehealth modalities for the delivery of healthcare has taken on a new urgency over the past nine months as the United States has had to adapt to societal measures aimed at mitigating the spread of the SARS-CoV-2 virus. Factors including aggressive social isolation measures as well as healthcare systems restrictions on in-person ambulatory patient visits and elective surgeries have led to the necessary adaptation of telehealth tools so that healthcare delivery and patient care could continue relatively unabated. The modification of pre-COVID-19 federal and state regulations on telehealth during the public health crisis has allowed for telehealth models to be created and employed in relatively rapid fashion [4]. Barriers to its application and full acceptance however likely still exist and may include primarily health care provider acceptance, patient familiarity with technology, internet access and broadband speed, dissatisfaction with the lack of full patient interaction, and privacy concerns amongst some patient cohorts [5]. Despite these barriers, widespread adoption in the medical community has occurred out of necessity during the pandemic, with very little evidence to date examining provider acceptance and satisfaction with telehealth as a healthcare model during the public health emergency.
The application of telehealth in the field of physical medicine and rehabilitation (PM&R), more specifically called telerehabilitation, has grown significantly in the past decade [6]. Via a variety of communication modes, including telephone, messaging, e-mail, and video conferencing, providers can evaluate and manage the medical needs of rehabilitation patients, including monitoring functional status and therapy progress, titrating medications for neurostimulation, neuropathic pain, or sleep, and troubleshooting neurogenic bowel and bladder management.
Some of the great advantages of telerehabilitation over conventional in-person rehabilitation medicine are the ability to observe the patient in their home context, share educational materials, and work on shared goal setting with various stakeholders without needing to have all relevant parties in the same location physically. It allows for more frequent check-in and reduces hassle for mobilityimpaired patients for whom transportation may be an issue, such as patients with spinal cord injury (SCI), who may live geographically further from the nearest spinal cord injury specialist [7].
Telerehabilitation also comes with a variety of challenges, including the need to protect patient privacy, as well as inability to perform physical examination. The latter is particularly relevant in the field of physical medicine and rehabilitation, in which physical examination is essential in making diagnoses and evaluating certain common conditions in rehabilitation patients, such as wounds, abnormalities of strength, sensation, coordination, and spasticity. As with all telehealth, telerehabilitation is also limited by the inability to perform procedures (joint injections, chemodenervation, etc.). However, telehealth modalities can still be quite useful to assess patients preand post-procedure.
Therapy services, such as occupational therapy, physical therapy and speech-language pathology, have taken similar positions on “telepractice”, a term used to avoid the misperception that telehealth services are offered only via a healthcare setting [8]. Each discipline encourages telepractice as long as the patient or client is receiving services equivalent to the quality of services they would receive in person and that the decision to use telepractice is consistent with adherence to the Code of Ethics, scope of practice, state and federal laws, and policies set forth by each discipline’s governing body [8-10]. Telepractice includes remote monitoring, teleconsultation, use of mobile apps, and both synchronous and asynchronous assessment and treatment platforms. Allied health’s concept of telepractice is equivalent to the more focused concept of telerehabilitation we discuss herein. While allied health professions are enthusiastic about telerehabilitation, its use in practice is not prevalent. Many argue that the technology developed faster than the environment in which it is to be used, leaving large gaps in user education, supporting infrastructure, and development of legal and regulatory requirements at state and federal levels [11]. Still, research indicates that when telerehabilitation is implemented in a supportive environment, it does appear to augment the balance between efficiency and clinical outcomes [12]. The COVID-19 pandemic has given rise to state-specific executive orders that allow for temporary flexibilities in allied health licensing and telerehabilitation, and this has emphasized both the challenges and the opportunities that allied health telerehabilitation presents [13]. Lessons learned during this time will hopefully serve to advance allied health telerehabilitation through development of telerehabilitation education standards, supportive infrastructure, and state laws that support the safety and privacy of clients while improving access to and efficiency of allied health services.
Telehealth for psychological services has been in continuous evolution since 1997, when the US Navy first started using telecommunication to conduct remote psychiatric interviews [14,15]. In rehabilitation psychology specifically, telehealth is primarily used for assessment, including neuropsychological testing, and for therapeutic interventions. Available methods for telehealth-based assessment include a broad variety of telephonic-based testing tools and batteries [16]. The COVID-19 pandemic has accelerated the evolution of teleneuropsychology (TeleNP), and the professional field of clinical neuropsychology in the United States has put forth existing practice recommendations and guidelines for TeleNP practice [17]. Telerehabilitation interventions in rehabilitation psychology are also coming into maturity. Telerehabilitation for mental health services has been considered since the 2000s to be a reasonable and efficacious way to reach patients who have problems accessing behavioral healthcare [15,18-22]. Overall, telerehabilitation psychology shows great promise across ages and diagnoses showing overall efficacy and patient and caregiver satisfaction [23,24].
Telerehabilitation in medicine, therapy, and psychology can improve access to healthcare services for those living remotely and for those with transportation barriers that prevent access to in person care, though adoption across disciplines has historically been slow and hindered by numerous barriers. The COVID-19 pandemic created a healthcare environment that suddenly became reliant on telehealth delivery, forcing not only health systems to rapidly adapt, but also rehabilitation providers with limited to no telerehabilitation experience to instantly shift to telerehabilitation. This unprecedented situation allows us the opportunity to probe the experiences and opinions of rehabilitation practitioners in medicine, therapy, and psychology who have adopted telerehabilitation during this time. This insight will inform the potential for wider scale adoption of telerehabilitation practices even after social distancing restrictions are lifted. To that end, the purpose of this study was 1) To assess the feasibility of rapid implementation of telerehabilitation in telehealthnaïve providers; 2) To determine rehabilitation providers’ perceptions of the usability of telerehabilitation; 3) To determine rehabilitation providers’ satisfaction with telerehabilitation; and 4) To determine which patient populations are more challenging to treat via telerehabilitation.
Methods
We conducted an anonymous closed survey study of rehabilitation providers at a single University Medical Center and an affiliated large urban county hospital. Study procedures were approved by the University Human Research Protections Office as exempt research. Inclusion criteria required that participants were rehabilitation providers fluent in English who used telehealth technology to provide clinical services between March 16, 2020 (the day that in-person clinical services were restricted at the Medical Center) and August 2020 (the last survey was collected on August 19, 2020). Survey invitations were sent via electronic REDCap™ link to a known group of 70 physicians (including PM&R attendings and residents), 3 advanced practice providers, 48 therapists (Physical Therapists, Occupational Therapists, Speech Therapists), 3 rehabilitation psychologists, and 2 other providers (rehabilitation counselor, physician assistant), totaling 126 providers. Survey participants were faculty and staff, and participation was voluntary, thus no written consent was obtained.
The survey (see Appendix A) included questions to capture demographic information (i.e., age, gender, race) and other provider characteristics (profession, previous telehealth experience, comfort using the internet), information about clinical populations the providers served, information about the telerehabilitation visits (primary reason for using telehealth, telehealth modality, problems during visits), and perceptions on the usability of telehealth [the Telehealth Usability Questionnaire (TUQ)]. The TUQ includes 5 subscales – Usefulness, Ease of Use, Effectiveness, Reliability, and Satisfaction – that captured overall usability of a telehealth system [25]. For this study, we used all but the 3-item Reliability subscale, for which two items had a high frequency of “not applicable” reported by providers; these items were related to making mistakes using the system and the system giving error message. We do report average scores for the remaining single item, “I think the visits provided over the telehealth system are the same as in-person visits.”
Statistical analyses were performed in IBM SPSS Statistics 26.0™ for Windows. To characterize the sample and to describe their experiences with telerehabilitation, we examined descriptive statistics, including means and standard deviations for continuous variables and frequencies and percentages for categorical variables. We also descriptively compared characteristics of telerehabilitation visits and telehealth usability and satisfaction by provider type (medical, therapy, psychology/other).
Results
Of 126 providers who received survey invitations, 68 were eligible and completed provider information for the survey (response rate: 54.0%). Of those, 4 did not complete the full survey, leaving 64 participants who completed through the TUQ (response rate: 50.8%).
Table 1 summarizes the descriptive characteristics of the sample (n=68), which represented a variety of rehabilitation providers. Notably, though everyone was “very comfortable” to “completely comfortable” using the internet, only 4.4% had previous telehealth experience. Despite almost all providers using telehealth for the first time and in the context of a rapid shift to telerehabilitation in response to the pandemic, they reported being very satisfied with telerehabilitation (5.81 out of 7) and found it to be useful (6.27 out of 7), easy to use (5.72 out of 7), and effective (5.33 out of 7). However, most did not agree (3.0 on a 1=disagree to 7=agree scale) that telerehabilitation visits were the same as in-person visits.
| Provider Characteristics (n=68) | n (%) | ||
|---|---|---|---|
| Age [Mean (SD)] | 39.0 (11.5) | ||
| Gender | |||
| Men | 22 (32.4) | ||
| Women | 46 (67.6) | ||
| Race | |||
| White, non-Hispanic | 43 (63.2) | ||
| White, Hispanic | 4 (5.9) | ||
| Black or African American, Hispanic | 1 (1.5) | ||
| Asian/Asian American | 18 (26.5) | ||
| Middle Eastern/North African | 2 (2.9) | ||
| Profession | |||
| Doctor/physiatrist (attending or resident) | 31 (45.6) | ||
| Nurse Practitioner or Physician Assistant | 4 (5.9) | ||
| Physical Therapist | 16 (23.5) | ||
| Occupational Therapist | 6 (8.8) | ||
| Speech Therapist | 3 (4.4) | ||
| Psychologist | 2 (2.9) | ||
| Counselor/Social Worker/Psychology Intern | 3 (4.4) | ||
| Other | 2 (2.9) | ||
| Previous telehealth experience | (4.4) | ||
| Comfort using the internet (1-10 scale) | |||
| Completely comfortable (10) | (63.2) | ||
| Very comfortable (7-9) | (36.8) | ||
| Telerehabilitation Visit Characteristics (n=67) | |||
| Primary reason visit was conducted via telehealth | |||
| COVID-19 restrictions | 61 (89.7) | ||
| Provider preference | 1 (1.5) | ||
| Patient preference | 5 (7.4) | ||
| How telerehabilitation visits were conducted (multiple responses) | |||
| Telephone audio only | 36 (52.9) | ||
| Computer audio only | 5 (7.4) | ||
| Computer audio & video | 53 (77.9) | ||
| Computer video & telephone audio | 20 (29.4) | ||
| Smartphone audio & video | 13 (19.1) | ||
| Modified clinic | 7 (10.3) | ||
| Experienced problems with telerehabilitation visit | 28 (41.2) | ||
| Technical problems | 23 (82.1) | ||
| Quality of technology | 9 (32.1) | ||
| Limitations of technology | 20 (71.4) | ||
| Cognitive issues (patient) | 12 (42.8) | ||
| Communication issues | 3 (10.7) | ||
| Physical issues (patient) | 1 (3.6) | ||
| Visual issues (patient) | 2 (7.1) | ||
| Billing/insurance | 5 (17.9) | ||
| Telehealth Usability Questionnaire± (n=63) | Mean (SD) | ||
| Usefulness | 6.3 (0.76) | ||
| Ease of use | 5.7 (1.05) | ||
| Effectiveness | 5.3 (1.03) | ||
| Satisfaction | 5.8 (1.03) | ||
| Think telehealth visits were the same as in-person | 3.0 (1.65) | ||
| Clinical Problems and Telerehabilitation (n=67) | |||
| Clinical Problem Addressed During Telerehabilitation Visit | n (%) | Especially challenging to treat using telehealth* | |
| Concussion | 22 (32.8) | 4 (18.2) | |
| Traumatic Brain Injury | 25 (37.3) | 11 (44.0) | |
| Stroke | 27 (40.3) | 10 (37.0) | |
| Spinal Cord Injury | 11 (16.4) | 1 (9.1) | |
| Amputation | 7 (10.4) | 1 (14.3) | |
| Traumatic Orthopedic Injury | 6 (9.0) | 1 (16.7) | |
| Chronic Orthopedic Injury | 17 (25.4) | 2 (11.8) | |
| Musculoskeletal Pain | 40 (59.7) | 18 (45.0) | |
| Multiple Sclerosis | 8 (11.9) | 1 (12.5) | |
| Guillain-Barré Syndrome | 2 (3.0) | 0 (0.0) | |
| Pelvic Disorder and/or Pain | 4 (6.0) | 4 (100.0) | |
| Urinary or Bowel Dysfunction | 7 (10.4) | 3 (42.9) | |
| Wound | 4 (6.0) | 4 (100.0) | |
| Burn Injury | 1 (1.5) | 1 (100.0) | |
| Other Chronic Pain | 12 (17.9) | 2 (16.7) | |
| Epilepsy | 5 (7.5) | 0 (0) | |
| *Percentage indicating yes out of the number of providers who reported addressing the specific clinical problem during a telehealth visit. ±Telehealth Usability Questionnaire subscales range from 1-7; 1=disagree to 7=agree. |
|||
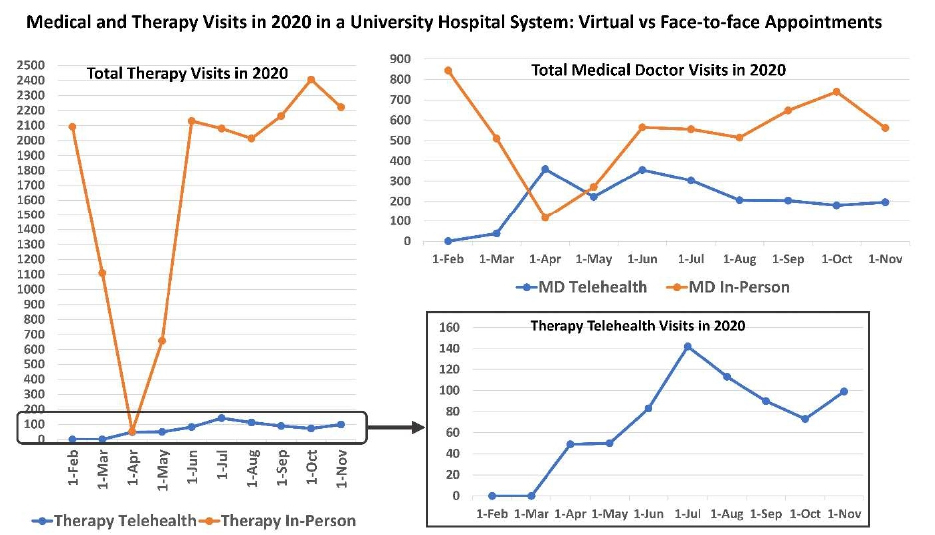
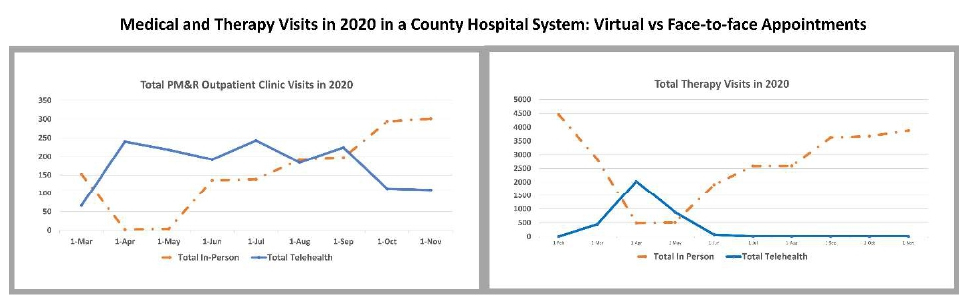
Figure 1 presents the total number of in-person versus virtual physician and therapy visits in the university hospital system from February to November of 2020. Figure 2 presents total number of in-person versus virtual physician and therapy visits in the county hospital system from February to November of 2020. For rehabilitation physicians, in-person encounters had a sudden dip from March to April with a gradual rise after through November. In more recent months, telehealth visits continued to constitute about 20% of all the visits for physicians in both the university hospital and the county hospital system ambulatory clinics. For therapy visits, the county system had some virtual visits in March through May, but they changed to in-person visits post May due to lack of video interface availability in the system. In the university system, virtual therapy visits continued to constitute about 4-5% of the total volume even after strict restrictions were lifted.
Figure 1: Medical and therapy visits in 2020 in a university hospital system: virtual versus face-to-face appointments.
Figure 2: Medical and therapy visits in 2020 in a county hospital system: virtual versus face-to-face appointments.
Table 1 also details the number and percentage of providers who indicated they worked with each clinical population and the number and percentage of providers who indicated that telerehabilitation was particularly challenging in each specific clinical population. Over one-third of practitioners treating patients with traumatic brain injury, stroke, musculoskeletal pain, pelvic disorder and/or pain, and/or urinary/bowel dysfunction found these conditions to be especially challenging to treat via telehealth modalities.
Table 2 presents telerehabilitation visit characteristics and TUQ scores by provider group, including Medical (physicians, residents, nurse/nurse practitioners, physician assistants), Therapists (occupational, physical, speech-language), and Psych/Other (neuropsychology, rehabilitation psychology, counselors, other) practitioners. Medical providers conducted telerehabilitation visits via telephone audio-only more often than others, with very few therapists conducting visits with telephone audio-only. Use of a modified clinic (patient in clinic but in a separate room from provider with communication via telehealth) was performed almost exclusively by psychologists for neuropsychological exams. Video teleconferencing utilized BlueJeansTM, a HIPAA-compliant software program that permits real-time audio-visual interaction between patients and rehabilitation providers. Beyond one-on-one interactions, video conferencing also allowed for delivery of services to groups of patients simultaneously, such as in our COVID Recover Wellness Group, a patient support group led by mental health professionals. Additionally, this format allowed for real time screen sharing to present slides or even a “whiteboard” to create original and more unique materials for the patient viewers. Finally, digital materials and resources (e.g., documents and files, website hyperlinks) could be shared directly with patients via the chat feature. Usability and Satisfaction scores were comparable across providers, though therapists disagreed the most with the statement that telerehabilitation and inperson visits are the same.
| Medical(n=35) | Therapists(n=25) | Psych/Other(n=7) | |
| Primary reason visit was conducted via telehealth COVID-19 restrictions Provider preference Patient preference |
34 (97.1) 0 1 (2.9) |
21 (84.0) 0 4 (16.0) |
7 (100.0) 0 0 |
| How telerehabilitation visits were conducted (multiple responses possible) Telephone audio only Computer audio only Computer audio & video Computer video & telephone audio Smartphone audio & video Modified clinic |
29 (82.9) 2 (5.7) 24 (68.6) 12 (34.3) 7 (20.0) 2 (5.7) |
2 (8.0) 0 23 (92.0) 5 (20.0) 3 (12.0) 0 |
5 (71.4) 3 (42.9) 6 (85.7) 3 (42.9) 3 (42.9) 5 (71.4) |
| Experienced problems with telerehabilitation visit Technical problems Quality of technology Limitations of technology Cognitive issues (patient) Communication issues Physical issues (patient) Visual issues (patient) Billing/insurance |
13 (37.1) 11 (84.6) 6 (46.2) 10 (76.9) 5 (38.5) 3 (23.1) 1 (7.7) 0 3 (23.1) |
10 (40.0) 8 (80.0) 2 (20.0) 8 (80.0) 3 (30.0) 0 0 0 2 (20.0) |
4 (71.4) 4 (100) 1 (25.0) 2 (50.0) 4 (100) 0 0 2 (50.0) 2 (50.0) |
| Telehealth Usability Questionnaire± | Mean (SD) | Mean (SD) | Mean (SD) |
| Usefulness Ease of use Effectiveness Satisfaction |
6.3 (0.66) 5.7 (0.89) 5.5 (1.08) 5.9 (1.01) |
6.1 (0.88) 5.7 (1.25) 5.1 (1.02) 5.7 (1.09) |
6.6 (0.78) 5.4 (1.00) 5.1 (0.72) 5.8 (1.02) |
| Think telehealth visits were the same as in-person | 3.1 (1.75) | 2.6 (1.58) | 3.7 (1.21) |
| ±TUQ Medical: n=33 Usefulness, n=32 Ease of Use and Satisfaction and telehealth vs in-person question; n=31 Effectiveness; TUQ Therapists: n=25 for all; TUQ Psych/Other: n=6 for all. Scores range from 1-7 with 1=disagree and 7=agree. |
|||
Discussion
Due to the pandemic, routine outpatient nonemergent care in the United States came to a standstill in mid- March 2020 in many healthcare systems until alternative measures could be established. In the state of Texas in response to the shutdown, both face-to-face and virtual encounters were deemed billable at the same level. Centers across the nation tried to set up and implement telehealth platforms with varying success. Platform needs varied based on the clinical setup, specialty, and type of practice. Services like psychology, counseling, and others that base their assessment on intake questionnaires and history could continue evaluation seamlessly, but specialties requiring hands-on examination, assessment, and/or treatment experienced challenges during virtual encounters.
At our university medical center, we used an integrated audio-video enabled interface imbedded in the electronic medical records system. For providers, the benefits of using this type of platform are security, ease of access, and hospital-based technical support. Providers reported that their patients, however, experienced platform access challenges, as the platform requires the use of a smart phone or computer and basic technical skills to install and run the application. If patients and providers working together were unable to solve technical issues on the patient’s end, the visit was converted to an audio-only telephone call. Video interface was not possible at the county hospital, so the visits were completed using audio-only telephonic encounters, which may explain the very low use of telehealth for therapy at the county hospital after strict restrictions were lifted. The audio encounters eliminated any technical challenges, but visual examination was not possible, therefore clinical reasoning was based mostly on the patient’s real-time report and medical history.
Though most providers agreed that telerehabilitation and in-person services did not offer the same experience and level of care, likely due to the inability to incorporate handson assessments and treatments during the visit, they did agree that telerehabilitation was useful, easy to use, and effective. We found that usability of and satisfaction with telerehabilitation did not differ based on provider type. Notably, almost all our respondents (95.6%) were firsttime telehealth users.
Our University and County health system data on inperson versus telehealth visits from February 2020 – before pandemic shutdowns occurred – through November 2020 – capturing more than one spike in Covid-19 cases – show that shifting to telerehabilitation can be done quickly and effectively. After strict shutdown orders were lifted, most therapy services returned to in-person, while medical doctor visits and psychology services continued to use telehealth modalities for a portion of total visits.
In addition to challenges with the types of services that cannot be easily provided via telerehabilitation, some diagnoses may be more challenging to treat virtually. Providers reported that patients with cognitive and speech impairments had difficulty using the telehealth platform, making telehealth encounters in these populations a challenge. However, complications were usually solved with assistance from the patient’s family and caregivers or the clinic support associates. Also, patients with musculoskeletal and pelvic pain needed more hands-on examination for diagnosis and management and thus reported limited benefit from virtual encounters.
As telehealth, and more specifically telerehabilitation, continues to evolve, it is important to note that multiple therapeutic telehealth options exist that may lessen the impact of the technical challenges of using telehealth for some patients with cognitive impairment, like those with TBI and stroke. For example, telephone-based problemsolving training interventions have demonstrated efficacy for improving outcomes for veterans with mild traumatic brain injury (TBI) [19], and telehealth cognitive rehabilitation interventions have shown efficacy for improving memory impairment after stroke [20]. Various telehealth options have also been validated for specialized cognitive assessment. Videoconference (VC)-based testing, modified from an in-person testing model, has been validated against traditional, in-person testing [30]. Overall, telerehabilitation psychology shows great promise, with studies in patients across ages and diagnoses showing overall efficacy and patient and caregiver satisfaction [23,24].
Our results parallel previous studies that showed favorable provider satisfaction for telehealth use in other disciplines [27-30]. Our good sample size of a heterogenous clinician group provides a broader idea of usability of telerehabilitation practice. As with many articles and commentaries from different individual specialties, we show that telehealth can be used in a rehabilitation setting and that it improves patient access to services during the pandemic.
The survey sample came from a single academic medical center, so generalization to all rehabilitation providers should be done cautiously. However, the respondents delivered telerehabilitation services in both the University Hospital clinics and the local County Hospital clinics, providing representation across these two distinct healthcare systems. The sample included a mixed group of physicians, therapists, psychologists, and counselors, so we cannot comment directly on experiences within specific professions. Though we know which subgroups of patients our providers found to be more challenging to treat using telerehabilitation, the details of how and why these clinical populations are more challenging were not collected and therefore require further study.
This study demonstrates that rapid implementation of telerehabilitation is feasible and easily adapted by telehealth-naïve providers. We also learned that all members of a rehabilitation team, including physicians, therapists, psychologists, and counselors, can use a single platform for telerehabilitation services, and that a telephone-only interface can be used if patients have technological or internet issues. While most providers reported that virtual encounters did not provide the same experience as face-to-face encounters, particularly when caring for patients with speech or cognitive deficits or muscular skeletal or pelvic pain, they were satisfied with the telehealth experience overall.
Author Disclosures
This abstract was presented as a poster at the Association of Academic Physiatrists (AAP) Annual Meeting, February 9-13, 2021 (Virtual). No funding was received for this study. No authors have conflicts of interest to report.
References
2. Stanberry B. Telemedicine: barriers and opportunities in the 21st century. Journal of Internal Medicine. 2000 Jun;247(6):615-28.
3. Buckner F. Telemedicine: the state of the art and current issues. The Journal of Medical Practice Management: MPM. 1998 Nov 1;14(3):145-9.
4. Patel PD, Cobb J, Wright D, Turer RW, Jordan T, Humphrey A, et al. Rapid development of telehealth capabilities within pediatric patient portal infrastructure for COVID-19 care: barriers, solutions, results. Journal of the American Medical Informatics Association. 2020 Jul;27(7):1116-20.
5. Almathami HK, Win KT, Vlahu-Gjorgievska E. Barriers and facilitators that influence telemedicine-based, realtime, online consultation at patients’ homes: systematic literature review. Journal of Medical Internet Research. 2020;22(2):e16407.
6. Galea MD. Telemedicine in rehabilitation. Physical Medicine and Rehabilitation Clinics. 2019 May 1;30(2):473-83.
7. Irgens I, Rekand T, Arora M, Liu N, Marshall R, Biering-Sørensen F, et al. Telehealth for people with spinal cord injury: a narrative review. Spinal Cord. 2018 Jul;56(7):643-55.
8. Association AS-L-H. Telepractice (Practice Portal), https://www.asha.org/Practice-Portal/Professional- Issues/Telepractice/ (Accessed October 5 2020).
9. Jana Cason DH, Kim Hartmann PhD OT, Tammy Richmond MS. Telehealth in Occupational Therapy. The American Journal of Occupational Therapy. 2018 Nov 1;72:1-8.
10. Association APT. Telehealth in Practice, https://www. apta.org/your-practice/practice-models-and-settings/ telehealth-practice/ (Accessed October 5 2020).
11. Heuer A, Hector JR, Cassell V. An update on telehealth in allied health and interprofessional care. Journal of allied health. 2019 Jun 6;48(2):140-7.
12. Reid DP. Practitioner Application: Hospital Value- Based Purchasing Performance: Do Organizational and Market Characteristics Matter?. Journal of Healthcare Management. 2018 Jan 1;63(1):48-9.
13. Lee AC. COVID-19 and the advancement of digital physical therapist practice and telehealth. Physical Therapy. 2020 Jul;100(7):1054-7.
14. James LC, Folen RA. Behavioral telehealth: Using telemedicine to expand behavioral medicine services. Journal of Healthcare Information Management. 1999 Jan 1;13(4):17-26.
15. Jerome LW, Zaylor C. Cyberspace: Creating a therapeutic environment for telehealth applications. Professional Psychology: Research and Practice. 2000 Oct;31(5):478.
16. Carlew AR, Fatima H, Livingstone JR, Reese C, Lacritz L, Pendergrass C, et al. Cognitive assessment via telephone: a scoping review of instruments. Archives of Clinical Neuropsychology. 2020 Dec;35(8):1215-33.
17. Bilder RM, Postal KS, Barisa M, Aase DM, Cullum CM, Gillaspy SR, et al. InterOrganizational practice committee recommendations/guidance for teleneuropsychology (TeleNP) in response to the COVID-19 pandemic. The Clinical Neuropsychologist. 2020 Nov 16;34(7-8):1314-34.
18. Stamm BH. Bridging the rural-urban divide with telehealth and telemedicine. 2003: 145:155.
19. Bell KR, Brockway JA, Fann JR, Cole WR, De Lore JS, Bush N, et al. Concussion treatment after combat trauma: development of a telephone based, problem solving intervention for service members. Contemporary Clinical Trials. 2015 Jan 1;40:54-62.
20. Lawson DW, Stolwyk RJ, Ponsford JL, McKenzie DP, Downing MG, Wong D. Telehealth delivery of memory rehabilitation following stroke. Journal of the International Neuropsychological Society. 2020 Jan;26(1):58-71.
21. Johnson EK, Fraser RT, Lashley S, Barber J, Brandling- Bennett EM, Vossler DG, et al. Program of Active Consumer Engagement in Self-Management in Epilepsy: replication and extension of a self-management randomized controlled trial. Epilepsia. 2020 Jun;61(6):1129-41.
22. Chemtob K, Rocchi M, Arbour-Nicitopoulos K, Kairy D, Fillion B, Sweet SN. Using tele-health to enhance motivation, leisure time physical activity, and quality of life in adults with spinal cord injury: A self-determination theory-based pilot randomized control trial. Psychology of Sport and Exercise. 2019 Jul 1;43:243-52.
23. Hilty DM, Ferrer DC, Parish MB, Johnston B, Callahan EJ, Yellowlees PM. The effectiveness of telemental health: a 2013 review. Telemedicine and e-Health. 2013 Jun 1;19(6):444-54.
24. Jenkins-Guarnieri MA, Pruitt LD, Luxton DD, Johnson K. Patient perceptions of telemental health: Systematic review of direct comparisons to in-person psychotherapeutic treatments. Telemedicine and E-Health. 2015 Aug 1;21(8):652-60.
25. Parmanto B, Lewis Jr AN, Graham KM, Bertolet MH. Development of the telehealth usability questionnaire (TUQ). International Journal of Telerehabilitation. 2016;8(1):3.
26. Caze T, Dorsman KA, Carlew AR, Diaz A, Bailey KC. Can You Hear Me Now? Telephone-Based Teleneuropsychology Improves Utilization Rates in Underserved Populations. Archives of Clinical Neuropsychology. 2020 Dec;35(8):1234-9.
27. Esposito S, Voccia E, Cantarelli A, Canali A, Principi N, Prati A, Parma COVID-19 Pediatric Working Group. Telemedicine for management of paediatric infectious diseases during COVID-19 outbreak. Journal of Clinical Virology. 2020 Aug;129:104522.
28. Madden N, Emeruwa UN, Friedman AM, Aubey JJ, Aziz A, Baptiste CD, et al. Telehealth uptake into prenatal care and provider attitudes during the COVID-19 pandemic in New York City: a quantitative and qualitative analysis. American Journal of Perinatology. 2020 Aug;37(10):1005- 14.
29. Parisien RL, Shin M, Constant M, Saltzman BM, Li X, Levine WN, Trofa DP. Telehealth utilization in response to the novel coronavirus (COVID-19) pandemic in orthopaedic surgery. The Journal of the American Academy of Orthopaedic Surgeons. 2020 Jun 1;28(11):e487-e492.
30. Cullum CM, Weiner MF, Gehrmann HR, Hynan LS. Feasibility of telecognitive assessment in dementia. Assessment. 2006 Dec;13(4):385-90