Abstract
Introduction: A national perinatal survey in France in 2016 showed that 12.2% of women have instrumentally assisted vaginal births with vacuum extraction used in 49.8% of cases, making it the most frequently used form of obstetrical assistance. The 2006 initial concept of the Icup® vacuum extractor was based on the development of a single-use device with a partially deformable cup to avoid any fetal scalp injury. However, owing to a significant rate of premature cup detachment, this first device required technical improvements which resulted in a new version: the Icup2® which obtained the CE label in February 2017. The main objective of this preliminary study was to assess the efficacy of this new obstetrical vacuum extractor.
Method: A preliminary retrospective observational study was undertaken in one hospital from February to October 2017. In our current practice, we use mainly Drapier-Faure’s obstetrical vacuum device Minicup®. We evaluated ICup2® through a descriptive study of quantitative and qualitative data and an analysis of its success rate as well as the rates of fetal scalp and perineal injuries.
Results: Fifty-eight assisted deliveries using the Icup2® were carried out by 9 experienced operators. The success rate of the Icup2® was 91.4 %. The premature cup detachment rate was 17.2%. No significant fetal scalp injury was noted.
Conclusion: This new low-cost and highly effective French device meets the required conditions for instrumentally assisted deliveries. Following this preliminary study, a prospective multi-centred comparative study will be conducted.
Keywords
Obstetrical vacuum device, Assisted instrumental delivery
Introduction
In France, as shown in the 2016 national perinatal survey [1], 12.2% of vaginal deliveries are instrumentally assisted. The vacuum extraction device is by far the most commonly used in instrumental deliveries (49.8% of the aforementioned assisted births), and it is an instrument that is easy to handle and has a relatively fast learning curve for the operators [2].
In France, the most commonly used vacuum extraction devices are the multi-use cup by Drapier-Faure (Minicup®) (Collin-Gentile-Drapier, Paris, France) and the single-use Kiwi Omnicup® suction Cup. The Minicup® is made of a rigid metal cup with a suction system which is independent of the traction system [3]. The main disadvantage of this vacuum device is that it must be sterilized and requires the use of a motor to create the vacuum. The Kiwi Omnicup® (Clinical Innovations, Heathrow, UK) is a single-use vacuum device with a rigid plastic cup connected to a hand pump for suction and traction [4]. The cost of this vacuum device, which is made in the USA, is relatively high (about 55 € excl. VAT).
The first version of the ICup® (Gyneas, Goussainville, France) was developed by Prof. Jean-Patrick Schaal (patented in 2006). The objective was to develop a singleuse vacuum device that would cause less trauma to the epicranium. Indeed, a review of the 2010 Cochrane Data Base [5] concluded that non-metallic (soft) cups were responsible for fewer lesions of the fetal scalp (RR = 0.6; 95% CI: 0.53-0.86) and cephalohematomas (RR=0.61; 95% CI/ 0.39-0.95). The aim was also to compete with the Kiwi® suction cup. The Icup® had a 5 cm diameter cup with a traction wire and a flexible suction hose connected to an electric motor. The lower part of the cup in contact with the fetal scalp was manufactured in flexible plastic (polyurethane) and therefore partially deformable. A 2015 multicenter randomized controlled study [6] comparing the clinical impact of the Icup® to that of the Minicup® found a higher detachment rate and instrument failure rate in the ICup® group: 35.6% vs. 7.1%, p=0.0001. However, obstetric anal sphincter injuries (OASIS) were less frequent with the ICup® (1.7% vs.5.0%; p=0.003).
The ICup2® was developed to improve the high detachment rates of the first version of the ICup while maintaining the noticeable perineal and fetal skull benefits.
The objective of this study was to demonstrate the proof of concept of the ICup2® by studying success rates as well as fetal scalp and perineal lesions.
Methods
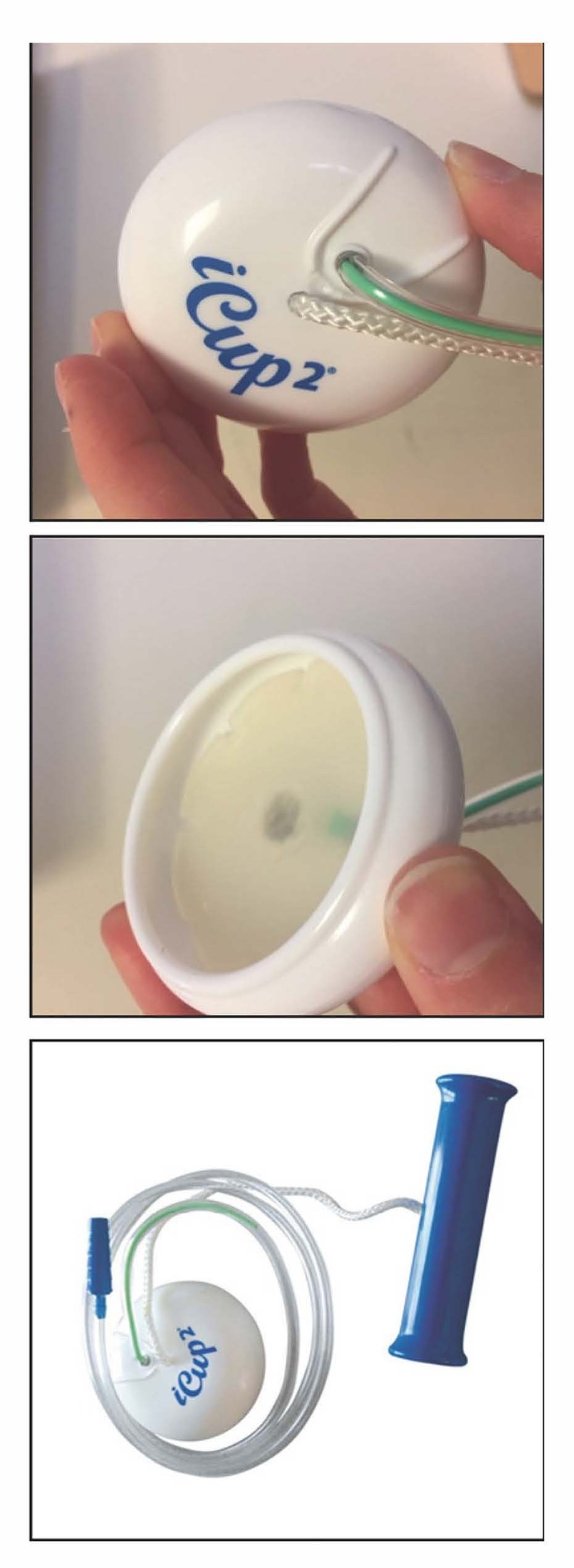
The ICup2® (Figure 1) is a sterile, single-use vacuum device designed in accordance with the required specifications of a modern vacuum extraction device [3], taking into account the advantages and disadvantages of the various vacuum devices currently available on the market. It is based on the same characteristics as the Minicup®, a sterilizable metal vacuum device for multiple use (cup shape, diameter 5 cm, height 1.5 cm).
Many improvements have been made to the ICup2® and take into account the needs of obstetricians : 1) effectiveness in limiting detachment (in vitro tests); 2) a smooth concave cup on the outside that is not traumatic for the mother, with an inner lip to improve adhesion and a silicone layer under the dome to prevent the vacuum access from being blocked by a blood clot; 3) the dome of the cup has a positioning notch allowing the operator to notice any intra-pelvic rotation during the progression; 4) a traction wire (15 cm) on the center of the dome of the cup which can be moved freely 180° around the frontal plane (thus avoiding jamming when detaching) and attached to a solid handle; 5) a suction system independent of the traction wire (length 1 m) lined with a 10 cm long green inner tube (corresponding to the height of the pelvic excavation) to avoid a plication which would prevent suction and to also serve as a marker which must always be partly visible (if no green colour is visible on the vacuum hose, the vacuum device is above the upper pelvic cavity) and ending with a variable diameter adapter designed to connect to the majority of vacuum pumps currently available.
The primary indications for the ICup2® are:
• Absence of fetal head progression in the pelvic cavity
• birth aid for ineffective pushing efforts
• Uterine inertia in spite of the use of oxytocine
• Fetal heart rate (FHR) abnormalities justifying instrumental assistance
The main contraindications to the application of the ICup2® suction cup common to other obstetrical vacuum devices are:
• Prematurity before 34 weeks of amenorrhea
• Frontal, breech, forehead and transverse (shoulder) presentations
• Incomplete cervical dilation
• A non-committed presentation, a variety of indeterminate positions
• The presence of a very large sero-blood bulge
• Too much asynclitism of the fetal head
• Hemorrhagic syndromes of the newborn, a disorder of fetal bone mineralization
• Maternal pelvic calluses, proven fetopelvic disproportion
• The suspicion of fetal macrosomia
• A dynamic or engaging dystocia
• The existence of fetal hypoxia
• A maternal-fetal infection
• A general anesthesia, a non-cooperative mother
• An inexperienced operator
Patients included were women aged 18 to 45 years, primiparous or multiparous, with cephalic presentation at term and obstetrical indications for instrumental assistance, respecting indications for the application of a vacuum device.
In the daily practice at our department, we use the metal Drapier-Faure Minicup®. The objective of this preliminary study was to demonstrate the proof of concept of the ICup2®. The longitudinal observational retrospective study was carried out in one medical centre. Data were collected over the period from February 2017 to October 2017. We analyzed 58 deliveries (non-consecutive) using an ICup2®, performed only by trained obstetricians (9 in number). Immediately after delivery, the operator noted information about the patient and the instrument-assisted delivery to reduce memory bias. All the data were recorded in our computer file (DIAMM® software). The information provided was the position of the head, the station of the head estimated clinically and ultrasonographically (presentation-to-perineum distance), the indication for the instrumental aid and its duration, the number of pulls, neonatal data (Apgar score, cordonal gas analysis, trauma to the fetal head), the number of detachments, the examination of the pelvic canal with the stages of perineal tears, possible complications and the satisfaction of the operator. The early neonatal status was also collected retrospectively to include the following information: neonatal transfer (resuscitation, neonatology, kangaroo unit), hospitalization in intensive care, pediatric examination at D1 and D3 looking for any complications in the fetal scalp and the rest of the general examination.
Figure 1. ICup2® , number CE1370.
Results
Out of our patients, 74% were primiparous with an average age of 30 years. All deliveries took place at term (between 37 weeks and 3 days and 42 weeks and 2 days). All patients received epidural analgesia except one for whom epidural analgesia was contraindicated due to a recent history of curatively anticoagulated deep vein thrombosis and who was on PCA (Patient Controlled Analgesia) morphine.
The instrumental deliveries were performed by 9 different operators (Assistants, Hospital Practitioners, University Professors).
Regarding the indications for instrumental aid (Table 1), 44.8% of cases are noted for no progression of presentation after 20 minutes of pushing efforts, and 53.4% for risk of fetal acidosis with an abnormal fetal heart rate. For the station and variety of positions of the head, these were systematically monitored clinically and ultrasonographically, and the station-perineal distance (SPD) was measured trans-perineally using the method described by Maticot et al. [7]. The majority of instrumental aids were used at the level of mid cavity (SPD between 21 and 40 mm).
| n (%) | |
| Primary indications | |
| Arrest of descent | 26 (44.8%) |
| Non-reassuring fetal status | 31 (53.4%) |
| Maternal indication | 1 (1.7%) |
| Station of the head | |
| Upper part | 17 (29.3%) |
| Middle part | 36 (62.1%) |
| Lower part | 5 (8.6%) |
| Position of the head | |
| OILA | 20 (34.5%) |
| OIRP | 13 (22.4%) |
| OIRA | 12 (20.7%) |
| OILP | 6 (10.35%) |
| OIRT | 2 (3.45%) |
| OILT | 1 (1.7%) |
| OA | 2 (3.45%) |
| OP | 2 (3.45%) |
| Number of pulls | |
| 1 à 3 | 38 (65.5%) |
| 4 à 6 | 20 (34.5%) |
| Duration of the procedure in min (minimum-maximum) | 6.32 (1-15) |
| Birth position | |
| OA | 52 (89.7%) |
| OP | 6 (10.3%) |
The efficacy of the ICup2® (Table 2) was analyzed in 2 ways: 1) success rate and 2) failure rate (use of another device and/or Caesarean section). The success rate (vaginal delivery with ICup2® alone) was 91.4%. Among 5 cases where the ICup2 failed (8.6%), one caesarean section was performed due to no progression of the head and suspicion of macrosomia and 4 cases of acceptable nonadherence of the ICup2® required a change of instrument (1 case to a metal cup and 3 others to Teissier’s spatulas). These problems of adhesiveness of the ICup2® cup were linked either to very dense fetal hair or to a significant sero-blood bulge. As a result of these instrument changes, all infants were born vaginally. It should be noted that in these failures there was one case of maternal myasthenia gravis and 1 case of fetal macrosomia at the high level of pelvic cavity. The overall detachment rate was relatively low (10/58; 17.2%), and vaginal delivery was possible in the majority of cases.
| n (%) | |
| Method of delivery | |
| Vaginal delivery by ICup2® alone = success | 53 (91.4%) |
| Failed ICup2®: instrument change and/ or caesarean section | 5 (8.6%) |
| Detachment followed by the use of another instrument | 4 (6.9%) |
| Caesarean section | 1 (1.7%) |
| Detachment of the cup (17.2 %) | 10 |
| 1 detachment | 4 |
| 2 detachments | 6 |
| Perineal lesions | |
| Périneum intact | 14 (24.1%) |
| Pseudo-intact* | 33 (56.9%) |
| 2nd degree perineal tear | 6 (10.35%) |
| OASIS | 2 (3.45%) |
| Episiotomy** | 4 (6.9%) |
Among the 53 successes, 88.7% of the vacuum deliveries were in Occiput-Anterior (OA) with 6 cases of detachment in Occiput-Posterior (OP) positions. When the initial position of the head was posterior (OILP, OIRP and OP), in 71.5% of cases we observed sufficient rotation of the head enabled by the ICup2® and a resulting vaginal birth in OA. The average duration of the procedure was 6.32 min.
Perineal data are detailed in Table 2. Four episiotomies were performed (6.9%) and 2 Obstetrical Anal Sphincter Injuries (OASIS) were regrettably registered (3.5%). These OASIS were of type 3a.
For the newborns (Table 3), the average weight was 3302 g (2301-4350), with 6 newborns weighing more than 4000 g (10.3%). These neonates had an Apgar score <7 after 5 minutes, of which only one had a pH<7.00. The latter was the only case requiring transfer to intensive care for respiratory distress and the outcome was favorable with discharge at D10. At 18 months, the child showed good psychomotor development and no learning difficulties. Regarding other neonatal hospitalizations: 12 children were transferred to the Kangaroo Unit (UK), including 4 for hypotrophy, 3 for monitoring following maternal pathologies (1 mother on beta-blockers, 1 myasthenic, 1 diabetic), 1 for desaturation with the discovery of a cardiac pathology (CAV), 1 for hypotonia and 2 for poor adaptation to ectopic life. All new-borns hospitalized in the UK were discharged following a reassuring pediatric examination.
No cephalohematoma or other scalp blisters were observed in the neonates. Only transient marks on the scalp were noted. No late complications were reported during post-natal consultations.
| n (%) | |
| Apgar score < 7 | |
| 1 min | 9 (15.5%) |
| 5 min | 3 (5.2%) |
| 10 min | 0 |
| Arterial pH | |
| < 7.20 | 28 (48.3%) |
| < 7.00 | 3 (5.2%) |
| Fetal Scalp | |
| Sero-blood bulge | 11 (19%) |
| Cephalohaematoma | 0 |
| Neonatal transfer | |
| Kangaroo Unit Stay | 12 (20.7%) |
| Transfer to neonatal intensive care | 1 (1.7%) |
Discussion
The ICup2® is a French design which is produced and assembled in France. The designers wanted a vacuum device that met the specifications for a modern vacuum device with the advantages of fewer fetal skull injuries from the use of non-metallic cups and a good quality/ price ratio. The main objectives of the 2006 modifications to the ICup® were to limit the number of failures and its lack of adhesion and consequent high detachment rate resulting from its deformability which was causing it to perform less well than the Minicup®. Cup detachment was therefore the desired improvement in the development of the ICup2®, with the aim of achieving a failure rate of less than 25% in order to be able to conclude that our new device is effective.
Our overall success rate of 91.4% of the 58 instrumental vacuum births was very satisfactory and in line with our expectations, and a very low C-section rate of 1.7% was noted. In comparison, the failure fate of the first ICup® (2006) was 35.6% compared to the 7.1% failure rate of the Minicup® in this randomized study [6]. A comparison made with the most widely used single-use suction cup in France, the Kiwi® suction cup, reveals that the Icup2® is at least as effective. Indeed, in a retrospective study from 2001, the Kiwi® suction cup used by a single team (that of its developer) had a success rate of 98% in 50 cases without any lesions of the fetal scalp [3].
Subsequently, in 2005 [9], a randomized study of 200 cases of instrumentally-assisted deliveries comparing the Kiwi® suction cup to « classic » metal suction cups showed a lower effectiveness of the Kiwi® with failure rates of 34% (versus 21%, OR = 1.9 [1.01-3.6]) and this difference persisted after adjustment for confounding factors (adjusted OR = 2.25 [1.01-5.0]). The caesarean section rate was identical in both groups [9.4% versus 8.2%, OR = 1.2 (0.4-3.2)], as was the rate of fetal scalp injury. However, there were more cases of jaundice in the “classic” suction group (2.3% versus 12.0 %, 0R = 0.18 [0.04-0.82] and adjusted OR = 0.10 [0.01-0.88]). Another randomized trial in 2006 [10], in which 206 Kiwi® assisted deliveries were compared to 198 so-called « conventional » vacuum device (n=198) assisted deliveries showed that the Kiwi® had a higher failure rate (30.1% versus 19.2% (RR 1.58 ; 95% CI : 1.10-2.24)) with more detachments (average 0.68 versus 0.28, and in 44% of cases versus 18% of cases with at least 1 detachment : p<0.0001) and a caesarean section rate of 8.3%. No difference was noted regarding severe maternal and fetal scalp blisters. It can therefore be said that in view of the results, the efficacy of the ICup2® is at least equal to the most commonly used single-use suction cup in France.
No case in our study has had more than 2 detachments. The possible explanations put forward by the operators for the detachment rate in our study (17.2%) were poor adhesion between the suction cup and a large amount of hair or a large sero-blood bulge. This detachment rate appears to be lower than in medical papers which report a rate of 22.3% with the Minicup® [5]. Only 4 cases of detachment resulted in a change of device (6.9%). In addition, the Icup2® is a very good device for aiding intra-pelvic rotation when placed on posterior or transverse varieties, with a successful occiput anterior rotation rate (occipitopubic release) of 75% (6/24), which corresponds to the results previously obtained with modern suction cups. In comparison, Equy et al. [6] found in their randomized study between 61.8% and 64.8% occiput anterior rotation of posterior and transverse varieties. The experience of the operators in our study will undoubtedly have had an impact on this data, since the correct placement of the cup is key to correct flexion and thus induced anterior rotation of the occiput.
Neonatal data are satisfactory in this situation of dystocic childbirth requiring the use of an instrument to assist the vaginal birth rate in level 3 maternity hospitals. Trauma to the fetal scalp appears to be low with the Icup2®, as no neonatal cutaneous or subcutaneous lesions were observed in this study. However, it is important to note again the operators were all experienced, which probably influenced this finding.
It has now been shown that the obstetric vacuum device is the instrument that causes the least maternal perineal trauma [11] and the CNGOF recommends that if a choice is possible, the vacuum device should be used [12]. In our study, the rates of perineal lesions were very low with 3.45% OASIS (2 cases) and a 6.9% episiotomy rate. Eighty-one percent of patients had an intact or pseudo-intact perineum (without muscle damage). In the study by Equy et al. [6], OASIS levels were 5% with the Minicup®; while in the randomized study by Attilakos et al. [9], OASIS levels were 7-8% ; and for Groom et al. [10], OASIS levels with the Kiwi® were 4.8% with an episiotomy rate of 61.7%. In a recent large retrospective study [13] of 1056 deliveries using vacuum extraction in a single highly experienced centre, the OASIS rate was 1.23%. It should be noted, however, that this very low OASIS level was achieved due to extensive use of the Couder’s maneuver for shoulder birth by this team [14,15].
Few studies have investigated learning curves in obstetrics. Regarding the obstetric suction cup, a French study on learning by residents has shown that the learning curve is relatively short and never more than 6 uses [2]. More recently, a model study aimed at analyzing the level of experience of 3 groups of operators and the traction forces they each applied showed a short learning curve and no difference in traction force between residents and experienced practitioners [16]. The handling of the ICup2® suction cup is similar to that of the Minicup® and how operators adapt to the device is easy. There is no difference in the success rate between the beginning and the end of the study. The ICup2® can be used without the need for specific training and it is easy to handle.
In terms of cost, an ICup2® suction device costs 35€, which is significantly less than other single-use suction cups on the market. The ICup2® is adaptable to all conventional vacuum motors - this allows centres which are already in possession of a motor to acquire this new device at no additional cost. Compared to multi-use suction cups, there are savings in sterilization and packaging costs.
Conclusion
The results of our preliminary study of 58 instrumentally assisted births suggest that the ICup2® meets the requirements for applicability and safety with an efficiency rate of 91.4%.
It is a new device which meets the requirements of the specifications of a modern suction cup, with the perineal and fetal scalp advantages associated with non-metallic suction cups. In addition, its cost is significantly lower than other single-use devices on the market.
As with any birth assistance instrument, it is essential that there is full compliance with the indications, operators must have understood, and mastered relevant techniques and the safety rules must be applied.
As a follow-up to this promising preliminary study, a prospective multi-centre study comparing the ICup2® with the multi-use Minicup® will be carried out.
Conflicts of Interest
Didier Riethmuller is the developer of ICup2®.
References
2. Velemir L, Vendittelli F, Bonnefoy C, Accoceberry M, Savary D, Gallot D. Courbe déapprenttissage de la ventouse obstétricale par les internes: étude préliminaire. Journal de Gynécologie Obstétrique et Biologie de la Reproduction. 2009 Sep 1;38(5):421-9.
3. Riethmuller D, Mottet N, Equy V (Eds). La ventouse obstétricale: un instrument moderne. Sauramps Médical 2019.
4. Vacca A. Operative vaginal delivery: clinical appraisal of a new vacuum extraction device. Australian and New Zealand Journal of Obstetrics and Gynaecology. 2001 May;41(2):156-60.
5. O’Mahony F, Hofmeyr GJ, Menon V. Choice of instruments for assisted vaginal delivery. Cochrane Database Syst Rev. 2010;(11):CD005455.
6. Equy V, David-Tchouda S, Dreyfus M, Riethmuller D, Vendittelli F, Cabaud V, et al. Clinical impact of the disposable ventouse iCup® versus a metallic vacuum cup: a multicenter randomized controlled trial. BMC Pregnancy and Childbirth. 2015 Dec 1;15(1):332.
7. Maticot-Baptista D, Ramanah R, Collin A, Martin A, Maillet R, Riethmuller D. Diagnostic échographique d’engagement de la présentation foetale. À propos d’une série prospective préliminaire française. Journal de Gynécologie Obstétrique et Biologie de la Reproduction. 2009 Oct 1;38(6):474-80.
8. Krispin E, Aviram A, Salman L, Chen R, Wiznitzer A, Gabbay-Benziv R. Cup detachment during vacuum-assisted vaginal delivery and birth outcome. Archives of gynecology and obstetrics. 2017 Nov 1;296(5):877-83.
9. Attilakos G, Sibanda T, Wintern C, Johnson N, Draycott T. A randomised controlled trial of a newhandheld vacuum extraction device. BJOG: An International Journal of Obstetrics & Gynaecology. 2005 Nov;112(11):1510-5.
10. Groom KM, Jones BA, Miller N, Paterson-Brown S. A prospective randomised controlled trial of the Kiwi Omnicup versus conventional ventouse cups for vacuumassisted vaginal delivery. BJOG: An International Journal of Obstetrics & Gynaecology. 2006 Feb;113(2):183-9.
11. Hamilton EF, Smith S, Yang L, Warrick P, Ciampi A. Third-and fourth-degree perineal lacerations: defining high-risk clinical clusters. American journal of obstetrics and gynecology. 2011 Apr 1;204(4):309.e1-6.
12. Riethmuller D, Ramanah R, Mottet N. Quelles interventions au cours du dégagement diminuent le risque de lésions périnéales? RPC Prévention et protection périnéale en obstétrique CNGOF. Gynécologie Obstétrique Fertilité & Sénologie. 2018 Dec 1;46(12):937-47.
13. Bourgon N, Mottet N, Bourtembourg A, Pugin A, Ramanah R, Riethmuller D. Lésions obstétricales du sphincter de l’anus et ventouse obstétricale chez des primipares à terme. Gynécologie Obstétrique Fertilité & Sénologie. 2018 Nov 1;46(10-11):686-91.
14. Mottet N, Bonneaud M, Eckman-Lacroix A, Ramanah R, Riethmuller D. Active delivery of the anterior arm and incidence of second-degree perineal tears: a clinical practice evaluation. BMC Pregnancy and Childbirth. 2017 Dec;17(1):1-8.
15. Hulot G, Ramanah R, Riethmuller D, Mottet N. The impact of active delivery of the anterior arm during vacuum-assisted vaginal delivery on perineal tears: a clinical practice evaluation. The Journal of Maternal-Fetal & Neonatal Medicine. 2019 Jan 31:1-5.
16. Eskander R, Beall M, Ross MG. Vacuum-assisted vaginal delivery simulation–quantitation of subjective measures of traction and detachment forces. The Journal of Maternal-Fetal & Neonatal Medicine. 2012 Oct 1;25(10):2039-41.