Abstract
Hamstring injuries are the most common pathology reported in professional soccer players and represent about 10-30% of all injuries. This study’s primary purpose was to identify specific injury patterns, location, and severity on MRI following acute hamstring injuries in a group of Major League Soccer (MLS) players. The secondary purpose was to present a new MRI classification protocol for identifying the location of hamstring injuries.
We retrospectively reviewed 19 MRIs ordered to evaluate suspected acute hamstring injuries during a period of 5 years. Intramuscular T2 hyperintensity was considered to represent muscle injury.
The long head of the biceps femoris was the injury site in 14 of 19 cases. It occurred in association with the semitendinous in four, semimembranous in one, and short head of the biceps in another of the injured athletes. Over half (11/19) of the reported cases sustained hamstring injuries that affected more than one muscle. A mean edema length of 10.6 cm was reported, with the severity of fiber disruption described as low in 7 (37%) and moderate in 12 (63%) of the 19 cases. We divided the total length of each muscle into 5 zones. The results demonstrate a prevalence of 14 cases affecting the distal Myotendinous junction.
The BFLH was the most commonly injured muscle in our cohort. Over half of the injuries were grade 2 fiber disruption severity, with no full-thickness injuries reported. This MRI classification allows a detailed muscle location and severity grading of acute hamstring injuries.
Keywords
Hamstrings injuries; Soccer; MRI; Biceps femoris
Introduction
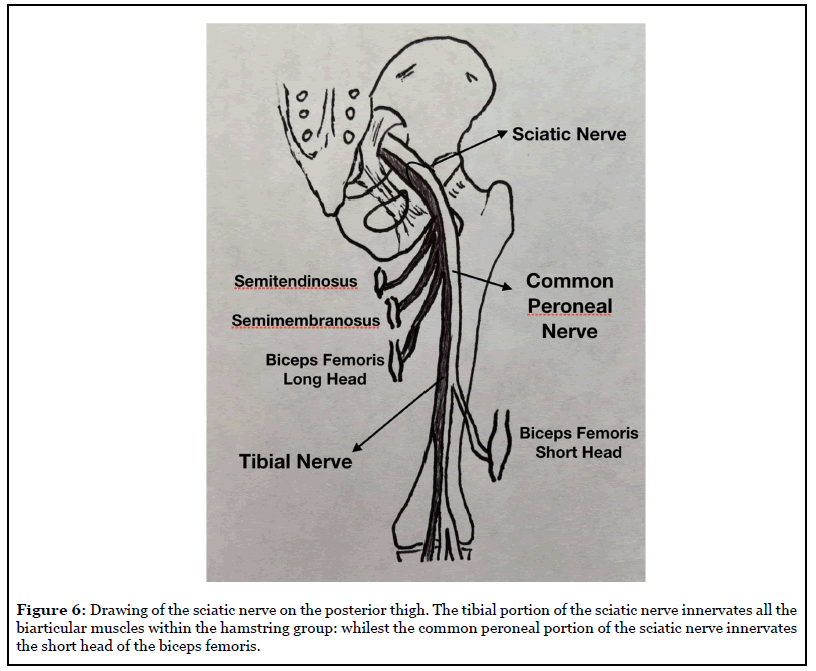
Hamstring injuries are the most common pathology reported in professional soccer players and represent about 10-30% of all injuries [1-3]. The hamstring complex is comprised of three muscles located in the posterior compartment of the thigh including the semimembranosus (SM), semitendinosus (ST), and biceps femoris (BF), which is comprised of the long head (BFLH) and short head (BFSH) [3-6]. Except for the BFSH, the hamstring consists of biarticular muscles spanning the hip and knee joints. They are largely responsible for both hip extension and knee flexion. Each one of these muscles has unique anatomic features and innervation patterns that make them susceptible to injury [7]. Regardless of the specific muscle involvement, they are collectively referred to as hamstring injuries [6-9].
The initial diagnosis of hamstrings injuries are commonly made clinically during the physical examination. However, ultrasound and MRI help optimize the diagnosis and are both equally sensitive in determining the presence of muscle injury [2,3,9-11]. While radiological findings have helped determine the precise location and grade of injury after a clinical suspicion of hamstring injury, only MRI findings have been correlated with prognosis and severity of the injury among elite professional athletes [10-13]. Additionally, MRI findings have not only been helpful in creating classifications for recovery time and risk of recurrence [1,3,9,14,15], but have also revealed a repeated pattern of incidence in professional soccer players [3,12,13]. A higher percentage of injuries affecting the BFLH compared to the other muscles of the hamstring complex has previously been reported, while the BFSH has demonstrated the lowest risk of injury [3,12,13].
Despite previous attempts to correlate MRI findings with prognosis for hamstring injuries, there is no accepted gold standard classification that unifies concepts regarding location, distribution and severity of injury. Having a detailed understanding of anatomy and common pathological findings would be beneficial for treating physicians to order and interpret hamstring related injuries on MRI. The primary purpose of this study was to identify specific injury patterns, location and severity on MRI following acute hamstring injuries in a group of Major League Soccer players (MLS). The secondary purpose was to present a new MRI classification protocol for identifying location of hamstring injuries.
Methods
Patient selection
A retrospective review of MRI’s for one MLS team was performed. The MRIs included were initially ordered to evaluate suspected acute hamstring injuries that occurred between January 2013 and December 2017. Inclusion criteria for the current study were as follows: 1) active roster player for Active roster player for FC Dallas team; 2) between the ages of 18 and 50 years who experienced a hamstring injury while participating in the MLS forum; and 3) required an MRI to assess the hamstring injury through the MLS injury protocol. Exclusion criteria were as follows: 1) subjects were not a member of MLS at the time of injury; 2) less than 18 years old or greater than 50 years old; 3) initial injury did not require an MRI to assess the hamstring; and 4) MRI images were unclear or unable to review due to quality. Mechanism of injury, timing of injury within the season (pre-season, early-season [first 1/3], mid-season [second 1/3], late-season [last 1/3], and playoffs), on-pitch position, leg dominance and re-injury rates were also reviewed. The current study was strictly data and outcome analysis through MRI review and did not require contact between the subject and the investigator. Consequently, there was not an opportunity to obtain informed consent as treatment had been completed and the subject was released from care for the injury. The Institutional Review Board of Texas Health Resources approved the research procedures (STU-2020-0764).
MRI technique
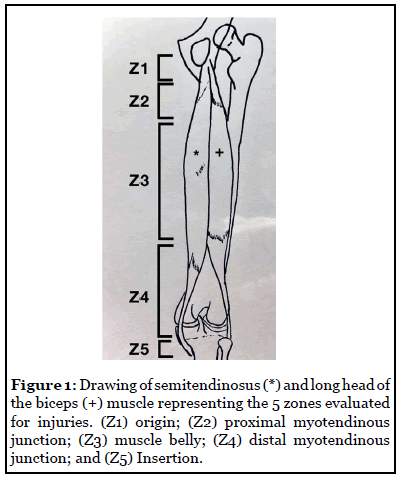
All athletes underwent a multiplanar sequence MRI. This protocol included 3 planes of fluid sensitive short tau inversion recovery T2 MR imaging in axial, coronal and sagittal planes. Images were independently interpreted by a fellowship trained musculoskeletal radiologist with more than five years of experience (NG), who described: muscle location, length and grade of visible edema, total length of the hamstring, distance from origin and insertion to injury, severity of fiber disruption (low, moderate or severe) (Table 1), and zones involved [6,12,16]. Zone involvement for each muscle was identified as the following: (Z1) muscle origin, (Z2) proximal myotendinous junction [MTJ], (Z3) muscle belly, (Z4) distal MTJ and (Z5) muscle insertion (Figure 1). Any additional findings deemed significant by the radiologist were also reported. The radiologist was blinded to clinical details and specific injury history.
| Fiber disruption | Description |
|---|---|
| Mild (Grade1) | No fiber disruption. Focal hyperintense signal with edema and hemorrhage about the musle or tendon fibers on T2-weighted and STIR sequences |
| Moderate (Grade 2) | Partial disruption of the muscle or tendon fibers. Hyperintense signal on T2- weighted sequences and a focal hematoma around and within fiber disruption. |
| Severe (Grade 3) | Complete disruption of the tendon or muscle fibers. T2 hyperintense signal occupying the injured area. If retraction focal fluid collection filling the gap and significant hematoma formation. |
Table 1: Traditional radiologic grade for strains based on MRI..
Statistical analysis
Descriptive statistics were evaluated for all hamstring injuries reviewed in the current study. Prevalence of primary muscle location was evaluated by the sample proportion value of a specific hamstring muscle being injured from the total number of hamstring injuries. Confidence intervals and significance testing were calculated for the single proportions of all four muscle locations (SM, ST, BFLH and BFSH). All data was analyzed using a common statistical software program (IBM SPSS Statistics, Version 25, Armonk, NY).
Results
Patient results
A total of 19 reported hamstring injuries were evaluated by MRI at an average of 16.6 (range 1-80) days from the initial injury. All patients were male with an average age of 25 (range 19-36) years. The most common player position for the current study were midfielders with 6 (56%) injuries, while the other affected positions included 2 (18%) center backs, 1 (9%) goalkeeper, 1(9%) full back and 1 (9%) right winger. Eight (42%) of the reviewed injuries occurred during the early-season, followed by 7 (39%) late-season and 4 (21%) mid-season injuries. No pre-season or playoff hamstring injuries were reviewed in the current study. Fifteen (75%) hamstring injuries were due to running, while 3 (16%) occurred during shooting and 2 (11%) injuries occurred during diving/ landing activities. A total of 11 (59%) injuries occurred on the right extremity, with 11 (59%) corresponding to the players’ dominant side. Overall, 5 athletes presented with a unilateral occurrence (3R,2L) while 2 athletes presented with bilateral hamstring injuries (2R,2L). One athlete reported a unilateral reinjury (2L – June to August 2014), while another athlete reported a cross-season/in-season unilateral reinjury (3R – September 2014, May to June 2015), and one athlete presented with a hamstring injury for 4 years in a row. (3R,1L – 2014-2017).
MRI results
On all MRI studies, intramuscular T2 hyperintensity was considered to represent muscle injury. Mild feathery interstitial signal hyperintensity limited to the muscle was scored as a low-grade tear. More defined linear signal abnormality corresponding to a partial thickness defect, with or without perifascial fluid, was scored as a moderategrade tear. Near complete defects of the muscle or MTJ, or complete disruption with retraction, was scored as a high-grade tear, which were not seen in our sample. No avulsion injuries and no complete tendon ruptures were present. Combined injury patterns involving more than one zone affected 15 (79%) of the 19 cases (Figure 2), with the 4 (21%) exceptions being an isolated injury to the distal attachment of the SM, another isolated injury to the muscle belly of the LHBF and two cases with injuries to the distal MTJ of the LHBF. A mean edema length of 10.6 cm (range of 3.0- 23.4 cm) was reported (Figure 3) with the severity of fiber disruption described as low in 7 (37%) and moderate in 12 (63%) of the 19 cases (Figure 4). Several secondary injuries were also reported including: T2 hyper intensity signal present as low to moderate edema of the mid aspect of the vastus medialis oblique and vastus lateralis muscle in 2 (10%) and 3 (15%) cases, respectively; 1 (5%) proximal iliotibial band syndrome; and 1(5%) rectus femoris strain.
Statistical results
Of the 19 reported hamstring injuries, a total of 25 muscles were involved. The distribution of hamstring muscle injury is shown in Table 2. Of these 25 muscle injuries, 14 (56%) occurred in isolation, while 11 (44%) involved more than one hamstring muscle. The BFLH was the most commonly reported site of injury in 14 of 19 cases (74%) and occurred in association with the ST in 4 (29%), SM in 1 (7%) and BFSH in 1 (7%) of the injured athletes. The sample proportion of BFLH as the primary location of injury for the 19 hamstring injuries was p=0.632 (95% CI = 0.415, 0.849) while the primary SM injury location demonstrated p=0.211 (95% CI=0.027, 0.395) and the primary ST injury location demonstrated p=0.105 (95% CI=-0.032, 0.242). The BFSH was only injured once in the 19 cases and was not diagnosed as the primary location of muscle injury (Figure 2). As demonstrated in Figure 5, there was a significant difference between confidence intervals for the BFLH and SM or ST. There was no significant difference between confidence intervals for the SM and ST.
Discussion
The main findings from the current study was that the BFLH was the primary location of hamstring muscle injury among a cohort of Major League Soccer players. The majority of injury patterns involved more than one zone, present in 15 (79%) of the 19 cases, and the most common grade of fibers disruption was moderate, observed in 12 (63%) of the 19 cases. The current study also successfully demonstrated MRI distribution and location of hamstring injuries in professional soccer players.
In contrast to other studies, in which the total length of each muscle is divided into 3 zones (proximal origin, muscle belly and distal insertion), the current study divided the total length of each muscle into 5 zones (proximal origin, proximal MTJ, muscle belly, distal MTJ and distal insertion). The results demonstrate a prevalence of 74% (14 cases) of the total hamstring injuries affecting the distal MTJ. This does not correlate with previous literature, in which hamstring injuries in athletes most commonly involve the proximal MTJ [13,17,18].
Injuries to the hamstring complex represent the most common lower extremity injury affecting professional soccer players [1-3]. The findings of the current study support the previously established international literature, specifically the high incidence of BFLH injury among soccer players. Cohen et al., reported on MRI findings in 38 professional football players who sustained an acute hamstring injury, and found that the BFLH was the most frequently injured muscle (25 of 38, 65.8%), with BFSH involved in only 5 cases (13.2%) and exclusively in distal injuries [12]. De Smet et al., reported on MRI findings in college athletes with acute hamstring injuries that 11 out of 15 injuries corresponded to the BFLH while none were attributed to the BFSH [13]. Slavotenik et al., found an 87% (26 out of 30 elite soccer players) incidence rate for injuries to the LHBF, and 17% (5 out of 30 cases) to the short head of the biceps [3]. Interestingly, injuries affecting the BF have been associated with faster recoveries than those involving the SM [6,19]. Anatomical features have been previously described and could justify the difference in prevalence of injury between the muscles of the hamstrings complex [4,6,7,20,21]. The BFSH is the only hamstring muscle that does not traverse the hip joint and is not innervated by the tibialis nerve, but instead from one or more motor branches originated from the common peroneal nerve or directly from the sciatic nerve (Figure 6) [3,4,7]. Therefore, the BFSH is exposed to less excursion and tension forces and has an independent nerve supply compared to the other three hamstring muscles that could explain with the lower incidence of injury.
The current study divided the total length of each muscle into 5 zones (origin, proximal MTJ, muscle belly, distal MTJ and insertion). This increase from the previously established literature enhanced the hamstrings muscles’ complex anatomy at the MTJ. Instead of having a narrow transition zone from muscle to tendon, the tendons of the hamstring extend into the muscle belly both proximal and distal to form the MTJ [13,22]. Due to the previous literature that demonstrates higher involvement of the intramuscular tendon during hamstring injury [3,12,13], this study separated injuries occurring to the MTJ from those affecting the muscle belly or the tendons’ origin and insertion. This division is important since it has been described that injuries affecting the tendon require a longer recovery period than those affecting the muscle fibers. In order for the tendon to restore its stiffness and function, required for strenuous activities such as sprinting, a remodeling phase of about 6 weeks is needed to enable the muscle to optimally recover for a faster return to function [14,23,24].
Results of the current study demonstrate a prevalence of 74% (14 cases) of the injuries affecting the distal MTJ, which parallels a previous study performed by Slavotinek [3]. In the current study the distal MTJ injury corresponded to the BFLH in 9 cases, SM in 3 cases and ST in 2 cases. Interestingly, this does not correlate with previous literature, in which hamstring injuries in athletes most commonly involve the proximal MTJ [13,17,18]. These findings might be explained by the small size of our sample, and not be a true representation of the prevalence of injury location in our soccer team. It is important to state that in previous studies that correlate MRI findings with severity of injury, the location of injury as proximal, central or distal within a muscle, did not affect the outcomes of the injury neither correlate with the number of games missed [3,12,14]. Instead, the difference in time missed from competition and higher reinjury rates have been associated with involvement of the tendon [14].
Other important findings in the current study, were that 11 players (44%) had more than one muscle involved. This has been correlated in previous literature with increased rehabilitation interval before returning to sports [12]. In the same way, the grade of fiber disruption and length of edema has been correlated with higher amount of time lost from competition [9,10,12,14]. In this study, the majority (65%) presented a moderated grade of fiber disruption, while no players had a full thickness disruption. The average length of edema was 10.6 mm (range of 3.0- 23.4 mm), which closely corresponds to a previous study that reported between 9.3 and 14.6 cm [12].
Several MRI classifications for location and severity of injury have been described [10,12-14,22], with one specifically categorizing hamstring injuries based on their anatomical site within the muscle and the extent of injury on MRI [14]. This study demonstrated a significant increase in time to return to sports and recurrence rates in those injuries that affected the tendon and those with higher grade of fibers disruption [14]. De Smet, described a very detailed classification, dividing the length of each muscle into eight segments (proximal and distal bone attachment, tendon, MTJ and muscle belly): however, all injuries affected the muscle belly or MTJ [13]. Another study demonstrated that the number of muscles affected (more than one) and muscle retraction was predictive of higher time lost from competition in professional football players and proposed an MRI scoring scale predictive of return to sports [12]. In a similar way, Slavotinek et al., reported that the volume of muscle injury and the extent of cross-sectional muscle involvement did correlate with prolonged rehabilitation time [3]. In our study we did not measure the cross-sectional area (CSA%). However, Gibbs et al., reported that the length of the edema on MRI had the strongest correlation with the rehabilitation interval and was faster and easier to report than CSA% [10].
While the current study does not comment on a return to soccer, future studies would benefit from the proposed MRI evaluation to further stratify time lost and a return to play. The authors believe that this is the first study reporting on hamstring injuries with MRI findings for an MLS team. Further studies are needed to define prevalence of injuries in MLS teams and create specific prevention plans and treating protocols to return athletes to sports in the safest way.
There are several limitations that need to be considered when interpreting the results of the current study. First, was that the current study population was limited to male professional soccer players. These findings may not necessarily reflect the injury characteristics within a more general population or at other levels of play. Second, this is a retrospective review of MRI findings in one MLS team. Ideally, a prospective study would predict the amount of time missed and determine the accuracy of our predictive model from the MRI. Additionally, we only had access to 19 MRI examinations which may not be representative of the prevalence of injuries amongst FC Dallas players during the study period. Third, there was no pre-established protocol for ordering an MRI study after an acute hamstring injury. This decision was based solely on the clinical expertise of the treating physician and medical staff. Lastly, the specific rehabilitation protocol and amount of time lost to competition was not reported. This is important in order to establish a prognostic classification, predicting the approximate time needed before going back to sports and the monetary cost for the team.
Conclusion
The BFLH was the most commonly injured muscle in the acute hamstring injuries for a MLS team during a period of 5 years. Over half (11/19) of the reported cases sustained hamstring injuries that affected more than one muscle. The average length of the edema was 10.6 cm and 65% of the injuries were grade 2 fiber disruption severity with no full thickness injuries reported. A majority (14/19) of the reported hamstring injuries primarily involved the distal MTJ. This MRI classification allows a detailed muscle location and severity grading of acute hamstring injuries.
Declaration of Interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Authors Agreement
All authors have seen and approved the final version of the manuscript being submitted. All authors warrant that the article is an original work, hasn’t received prior publication and isn’t under consideration for publication elsewhere.
References
2. Ekstrand J, Healy JC, Waldén M, Lee JC, English B, Hägglund M, et al. Hamstring muscle injuries in professional football: the correlation of MRI findings with return to play. British Journal of Sports Medicine. 2012 Feb 1;46(2):112-7.
3. Slavotinek JP, Verrall GM, Fon GT. Hamstring injury in athletes: using MR imaging measurements to compare extent of muscle injury with amount of time lost from competition. American Journal of Roentgenology. 2002 Dec;179(6):1621-8.
4. Arner JW, McClincy MP, Bradley JP. Hamstring injuries in athletes: evidence-based treatment. JAAOS-Journal of the American Academy of Orthopaedic Surgeons. 2019 Dec 1;27(23):868-77.
5. Malliaropoulos N, Papacostas E, Kiritsi O, Rad PM, Papalada A, Gougoulias N, et al. Posterior thigh muscle injuries in elite track and field athletes. The American Journal of Sports Medicine. 2010 Sep;38(9):1813-9.
6. Rubin DA. Imaging diagnosis and prognostication of hamstring injuries. American Journal of Roentgenology. 2012 Sep;199(3):525-33.
7. Woodley SJ, Mercer SR. Hamstring muscles: architecture and innervation. Cells Tissues Organs. 2005;179(3):125-41.
8. Askling C, Karlsson J, Thorstensson A. Hamstring injury occurrence in elite soccer players after preseason strength training with eccentric overload. Scandinavian Journal of Medicine & Science in Sports. 2003 Aug;13(4):244-50.
9. Hamilton B, Valle X, Rodas G, Til L, Grive RP, Rincon JA, et al. Classification and grading of muscle injuries: a narrative review. British Journal of Sports Medicine. 2015 Mar 1;49(5):306.
10. Gibbs NJ, Cross TM, Cameron M, Houang MT. The accuracy of MRI in predicting recovery and recurrence of acute grade one hamstring muscle strains within the same season in Australian Rules football players. Journal of Science and Medicine in Sport. 2004 Jun 1;7(2):248-58.
11. Connell DA, Schneider-Kolsky ME, Hoving JL, Malara F, Buchbinder R, Koulouris G, et al. Longitudinal study comparing sonographic and MRI assessments of acute and healing hamstring injuries. American Journal of Roentgenology. 2004 Oct;183(4):975-84.
12. Cohen SB, Towers JD, Zoga A, Irrgang JJ, Makda J, Deluca PF, et al. Hamstring injuries in professional football players: magnetic resonance imaging correlation with return to play. Sports Health. 2011 Sep;3(5):423-30.
13. De Smet AA, Best TM. MR imaging of the distribution and location of acute hamstring injuries in athletes. American Journal of Roentgenology. 2000 Feb;174(2):393- 9.
14. Pollock N, Patel A, Chakraverty J, Suokas A, James SL, Chakraverty R, et al. Time to return to full training is delayed and recurrence rate is higher in intratendinous (‘c’) acute hamstring injury in elite track and field athletes: clinical application of the British Athletics Muscle Injury Classification. Brnitish Journal of Sports Medicine. 2016 Mar 1;50(5):305-10.
15. Valle X, Alentorn-Geli E, Tol JL, Hamilton B, Garrett WE, Pruna R, et al. Muscle injuries in sports: a new evidence-informed and expert consensus-based classification with clinical application. Sports Medicine. 2017 Jul 1;47(7):1241-53.
16. Shelly MJ, Hodnett PA, MacMahon PJ, Moynagh MR, Kavanagh EC, Eustace SJ, et al. MR imaging of muscle injury. Magnetic Resonance Imaging Clinics. 2009 Nov 1;17(4):757-73.
17. Petersen J, Thorborg K, Nielsen MB, Skjødt T, Bolvig L, Bang N, et al. The diagnostic and prognostic value of ultrasonography in soccer players with acute hamstring injuries. The American Journal of Sports Medicine. 2014 Feb;42(2):399-404.
18. Hallén A, Ekstrand J. Return to play following muscle injuries in professional footballers. Journal of Sports Sciences. 2014 Aug 9;32(13):1229-36.
19. Balius R, Bossy M, Pedret C, Capdevila L, Alomar X, Heiderscheit B, et al. Semimembranosus muscle injuries in sport. A practical MRI use for prognosis. Sports Medicine International Open. 2017 May;1(3):E94.
20. Mendez-Villanueva A, Suarez-Arrones L, Rodas G, Fernandez-Gonzalo R, Tesch P, Linnehan R, et al. MRIbased regional muscle use during hamstring strengthening exercises in elite soccer players. PLoS One. 2016 Sep 1;11(9):e0161356.
21. Chumanov ES, Heiderscheit BC, Thelen DG. Hamstring musculotendon dynamics during stance and swing phases of high speed running. Medicine and Science in Sports and Exercise. 2011 Mar;43(3):525.
22. Garrett JW, Rich FR, Nikolaou PK. Computed tomography of hamstring muscle strains. Medicine and Science in Sports and Exercise. 1989 Oct;21(5):506-14.
23. Järvinen TA, Järvinen TL, Kääriäinen M, Kalimo H, Järvinen M. Muscle injuries: biology and treatment. The American Journal of Sports Medicine. 2005 May;33(5):745-64.
24. James R, Kesturu G, Balian G, Chhabra AB. Tendon: biology, biomechanics, repair, growth factors, and evolving treatment options. The Journal of Hand Surgery. 2008 Jan 1;33(1):102-12.
