Abstract
Background: Despite practice guidelines, strategies for lowering LDL-C are often poorly adopted in clinical practice.
Materials and Methods: Five countries (Brazil, Kuwait, Mexico, Saudi Arabia, and UAE) enrolled 2,422 patients with atherosclerotic cardiovascular disease (ASCVD) or familial hypercholesterolemia (FH) with low density lipoprotein cholesterol level (LDL-C) above 1.4 mmol/L. Patients were followed at 6 ± 2 months intervals to assess LDL-C level and treatment with ezetimibe and/or proprotein convertase subtilisin/kexin type 9 inhibitor (PCSK9i).
Results: 2422 patients 60.4 ± 11.7 years old and 29% women were enrolled from 87 participating cardiology sites. Overall, 91.1% of patients had coronary artery disease and FH in 12.3%. At baseline LDL-C was 2.96 ± 1.36 mmol/L and 1.87 ± 1.28 mmol/L (p<0.0001) at last available observation (n=2014). Proportion of patients achieving LDL<1.4 mmol/L (primary endpoint) increased from zero to 41.4% (p<0.0001).
At baseline, 99.2% of patients were on statin (81.3% high intensity statin), 34.4% on ezetimibe and its use increased significantly (62.9%, p<0.0001). PCSK9i use increased to 35.0% from baseline to last follow up (p<0.0001). Clinical outcomes such as ACS, CVA/TIA, PCI, CABG, or hospitalization for ASCVD reasons were recorded in 10.7% of patients during the follow up. Patients with no event had an overall LDL-C of 1.90 ± 1.3 mmol/L while those with an event had LDL-C significantly higher at the visit immediately prior to event (2.70 ± 1.35, p=0.0001).
Conclusion: The results indicate the feasibility of overcoming treatment inertia and improving LDL-C control which should help to achieve reduction in cardiovascular morbidity and mortality in ASCVD patients.
Keywords
Treatment inertia, Lipid lowering, Secondary prevention
Introduction
Low-density lipoprotein cholesterol (LDL-C) is a well-established risk factor for cardiovascular (CV) disease and there is considerable evidence that lowering LDL-C reduces the risk of both cardiovascular events and mortality in patients with CV disease [1]. Despite clear and concise guidelines [2], strategies for lowering LDL-C are often poorly adopted in clinical practice, and many patients fail to reach guideline-recommended levels despite physician education and quality improvement programs [3]. This care gap or treatment inertia, defined as the difference between evidence-based approach and real life, results in a significant burden [4] of atherosclerotic cardiovascular disease (ASCVD). Current guidelines recommend the use of high intensity statins as the first step [2,5,6]. Although statins remain the mainstay of dyslipidemia management, attainment of the recommended low density (LDL-C) or non-high density (non-HDL-C) lipoprotein cholesterol goals can be difficult even with the use of the highest doses of high intensity statin therapy [7,8]. To address this gap, clinical practice guidelines (CPG) now recommend addition of either ezetimibe or proprotein convertase subtilisin/kexin type 9 inhibitor (PCSK9i) or both based on clinical trial evidence [9-11].
Recent experience [12-14] indicated three different but interconnected levels of care gap; absence of cholesterol panel results on the chart in approximately 50% of patients, use of guideline recommended lipid lowering therapy in only a minority of patients and lowering of the LDL-C or non-HDL-C to recommended levels in approximately a third of patients with ASCVD. We, therefore, studied whether physician focussed, guideline-based patient level educational intervention can improve lipid lowering management as part of this international quality improvement (QI) program with educational intervention based on feedback to physicians on their management of dyslipidemia to support their decision making and choice of therapy in order to more optimally achieve guideline-recommended LDL-C level in ASCVD patients [2].
Materials and Methods
Cardiologists or internal medicine specialists from five countries (Brazil, Kuwait, Mexico, Saudi Arabia, and UAE) were invited to participate by the country principal investigator using the protocol and electronic data collection form developed by the Canadian Heart Research Centre and registered on ClinicalTrials.gov site (https://clinicaltrials.gov/ct2/show/NCT03861533?term=GOAL+International). In each country the study was approved by central ethics and/or by institutional review boards (IRB) as required. All patients signed an approved consent form in their language of choice addressing safety of participation and lipid lowering. Adverse events were not collected; participating physicians were encouraged to report adverse events as required in each country.
Inclusion criteria included men or women older than 18 years of age with either atherosclerotic cardiovascular disease (ASCVD) or familial hypercholesterolemia (FH). ASCVD was defined as one or more of coronary artery disease (history of acute coronary syndrome, myocardial infarction, percutaneous coronary intervention, coronary artery bypass grafting, or coronary stenosis >50% associated with stable angina), cerebrovascular disease (history of cerebrovascular accident or transient ischemic attack or carotid surgery), abdominal aortic aneurysm (history of surgery or percutaneous intervention) or peripheral arterial disease (history of surgery or percutaneous intervention). The FH was defined as LDL-C > 5 mmol/L prior to lipid lowering therapy and one of typical physical findings (stigmata) such as tendon xanthomata, xanthelasma, or arcus cornea, or personal or family history of early cardiovascular disease or of marked hyperlipidemia. All patients were receiving optimal (maximal or maximal tolerated) statin therapy for at least 3 months prior to patient enrolment and had LDL-C within the past 6 months above recommended level according to the most up-to-date Guidelines despite maximally tolerated statin therapy ± ezetimibe (or other lipid lowering therapy).
The exclusion criteria were current treatment with PCSK9i, current participation in another investigational study, or prior participation in the GOAL program.
Patients were enrolled on the date of signing the consent (Visit 1) and were then followed three more times (Visits 2, 3, and 4) with approximate intervals of 6 ± 2 months. The program started in the first part of 2019 and all follow up ended at the end of 2022. During the follow up visits the vital status was ascertained and occurrence of ASCVD events was captured and cholesterol panel was obtained (LDL-C measurement was mandatory in order to complete the visit).
The primary endpoint was proportion of patients achieving country specific guideline-recommended LDL-C levels after 18-month final visit or last available observation during follow up visits. The secondary endpoint was relative and absolute reduction of LDL-C with lipid lowering medications added during the observation period.
The intervention studied was physician education based on European guidelines [2]. The educational intervention was applied after each visit based on data entered. Specifically, physician was recommended to add LDL-C lowering therapy as recommended [2]. If the management chosen was consistent with the recommendations (2] then no further intervention was applied. If the management chosen was not consistent with the recommendation, physicians were alerted to that as an extra screen shown in the data collection form and asked if they would modify their management and if not to provide the most significant single reason as to why not such as co-morbidities, cost, not needed, patient refusal, patient intolerant, patient is on PCSK9i, or patient will return for Rx/will provide prescription next visit. The response “will return for Rx/will provide prescription next visit” was considered as actionable, and those patients were compared to others with respect to the primary and secondary outcomes.
The primary endpoint was proportion of patients achieving the CPG [2] recommended level for LDL-C at the last available follow up visit. The study was approved by central and institutional Review Ethics Board where appropriate, and all enrolled patients provided informed consent.
Invitations to participate were sent to the country Principal Investigator for each of the five participating countries: Brazil, Kuwait, Mexico, Saudi Arabia, and UAE.
The overall enrolment target for the program was minimum of 2,000 and maximum of 2500 patients based on the results of the GOAL Canada [3] with approximately 100 sites expected to enroll patients.
Statistical analysis
Continuous data are shown as means with standard deviation and categorical data as frequencies and percentages. Group comparisons were made using the chi squared test and t-test or Kruskal-Wallis test for discrete and continuous variables, respectively, where appropriate. Generalized mixed effect model for repeated measures analysis was performed in univariate and multivariable regression to determine the outcome across the visits. We considered the clustering of countries and hospitals within country in the random effect model. Compound symmetry structure was used for the variance covariance matrix. A value of p <0.05 was considered significant for all tests. All statistical analyses were performed in SAS software version 9.4 (SAS Institute, Cary, North Carolina).
Results
At the closing of the study (December 31st, 2022), 2,422 patients from 87 sites were enrolled with mean age of 60.4 ± 11.7 years and 29% were women. The country specific enrollment (proposed / achieved/number of sites) was: Saudi Arabia 480/662/26, Mexico 400/584/21, Brazil 400/498/18, Kuwait 400/405/8, and UAE 320/273/14.
The mean blood pressure was 129 ± 18 mmHg systolic and 75 ± 11 mmHg diastolic, heart rate of 72 ± 11 beats per minute, body mass index of 29.4 ± 5.3 kg/m² and waist circumference of 100.8 ± 14.0 cm.
Overall, 91.1% of patients had coronary artery disease, 8.3% had cerebrovascular disease, and 6.5% had peripheral arterial disease. FH was recorded in 12.3%, diabetes mellitus in 51.7%, hypertension in 73.2%, chronic kidney disease in 9.8%, smoking (current or past) in 51.7%, heart failure in 12.6%, atrial fibrillation in 6.7%, cancer in 1.9% and liver disease in 0.9%.
Cardiovascular medications, other than lipid lowering were aspirin (86.8%), renin-angiotensin system inhibitors (69.7%), beta blockers (75.5%), calcium channel blockers (24.2%), diuretic (25.8%), and oral anticoagulation (8.7%).
The LDL-C level at entry (Visit 1) was 2.96 ± 1.36 mmol/L with the range of 2.84 ± 1.64 mmol/L in Brazil and 3.31 ± 1.28 mmol/L in Saudi Arabia (p<0.0001). At the last available observation (n=2014) the LDL-C fell to 1.87 ± 1.28 mmol/L overall (Figure 1) and the range of 1.20 ± 0.74 mmol/L in Kuwait and 2.50 ± 1.49 mmol/L in Brazil (p<0.0001). Proportion of patients achieving an LDL<1.4 mmol/L (primary endpoint) increased significantly Figure 2 from zero in visit 1 to 41.4% at the at the 4th visit (p<0.0001) with the range of 73.1% in Kuwait and 14% in Brazil (p<0.0001). Proportion of patients achieving an LDL<1.8 mmol/L increased significantly from 11.4% at baseline to 55.2% overall at last available follow-up (p<0.0001).
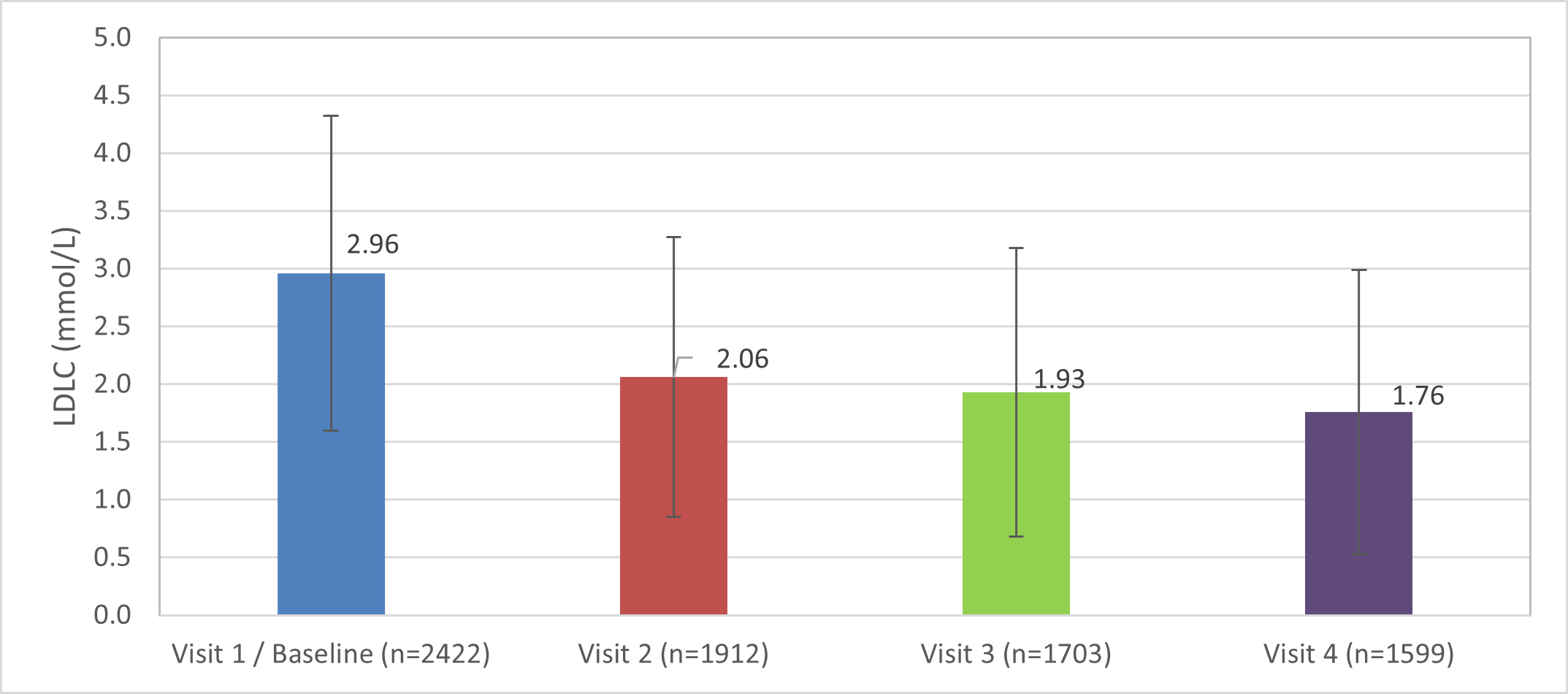
Figure 1. Reduction in LDL-C level (mean ± SD) from baseline to follow up using repeated measures of analyses (p<0.0001).
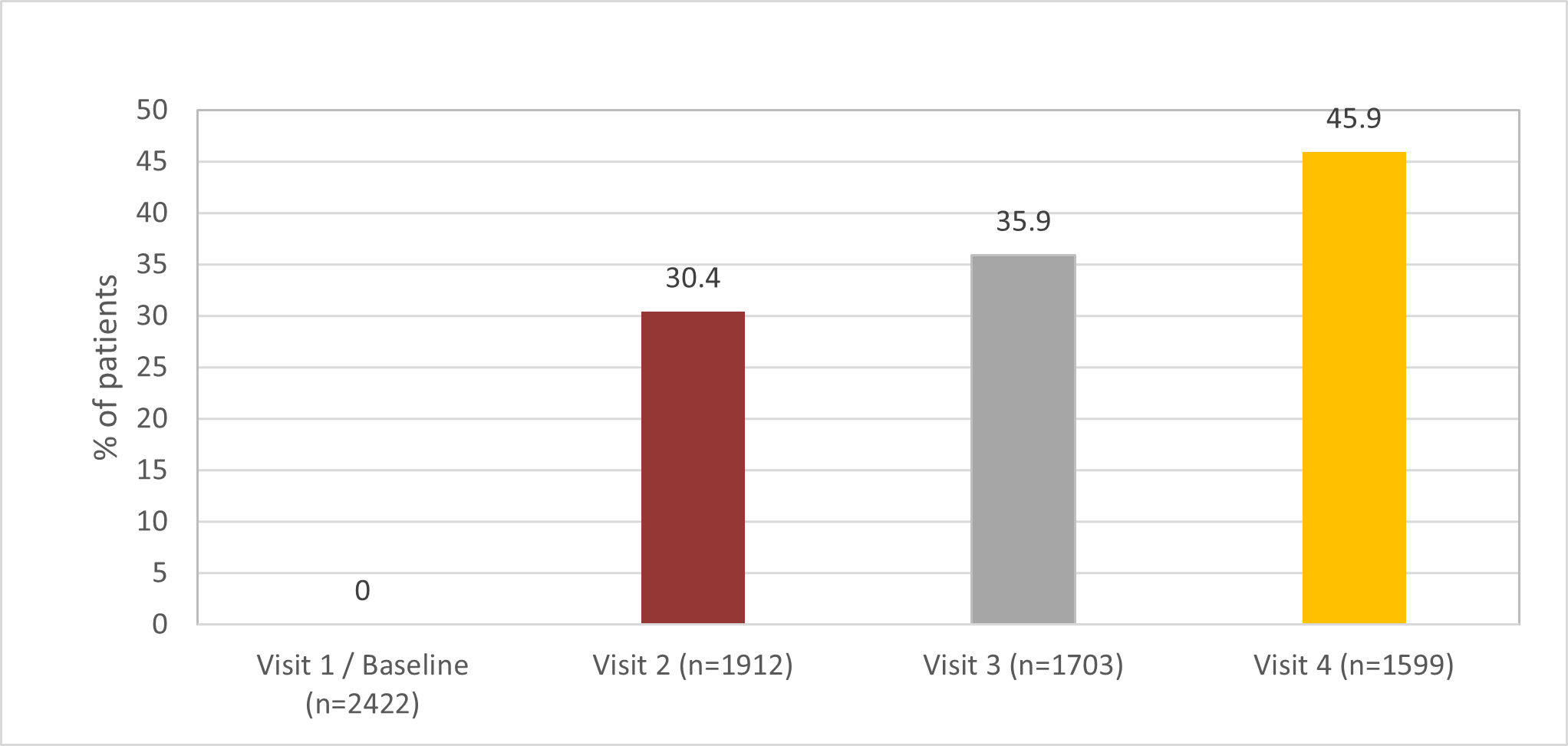
Figure 2. Proportion of patients achieving LDL-C of < 1.4 mmol/L (primary endpoint) from baseline to follow up (p<0.0001).
In visit 1, 99.2% of patients were on statin (81.3% were on high intensity statin) with very little difference between the countries and the use of statin remained high (97.6%) during the last available follow up. The use of ezetimibe was 34.4% (visit 1) with the range of 42.1% in UAE and 21.2% in Mexico (p<0.0001) and its use increased significantly (p<0.0001) across follow up visits: visit 2 (58.4%), visit 3 (62.9%), and visit 4 (66.3%) and with the last visit range from Mexico (73.7%) to Saudi Arabia (49.2%, p<0.0001). PCSK9i was not used prior to Visit 1 since it was an exclusion criterion. The use of PCSK9i rose significantly (p<0.0001) with follow up: Visit 2 (31.4%), visit 3 (36.1%), and visit 4 (37.2%) and with the range of 84.1% in Kuwait and 0.2% in Brazil (p<0.0001) on last visit. The use of other lipid lowering therapies (fibrates, niacin, bile acid sequestrants) was minimal (less than 6%) and did not vary across follow up visits (data not shown).
Overall, in the regression model adjusted for high intensity statin, lowering of the LDL-C level was driven significantly by addition of PCSK9i (estimate -0.65, p<0.0001) but not ezetimibe (estimate -0.12, p=0.06). Willingness to use PCSK9i at baseline as compared to not, was associated with a significant LDL-C level reduction at last available follow up (1.52 ± 1.29 vs 2.10 ± 1.22 mmol/L, p<0.0001). The benefit of PCSK9i addition was limited to countries where it was used and was not significant in Brazil or Mexico (used in 0.2% and 2.8% of patients respectively).
The most common reason for not prescribing ezetimibe at the last available follow up was cost (44.7%) with the range of 62.2% in Brazil and zero in Kuwait or UAE. The other reasons for not adding ezetimibe were addition not needed (21.3%), patient refusal (11.4%), and less than 10% each in patient intolerance, and patient is already on PCSK9i. About 15.0% responded that ezetimibe will be prescribed next visit or patient will be given prescription immediately. The most common reason for not prescribing PCSK9i was cost (62.2%) followed by not needed (17.9%) or patient refusal (9.1%). About 10% of physicians responded that PCSK9i will be prescribed next visit or patient will be given prescription now. Proportion of patients achieving LDL-C <1.4 mmol/L was significantly greater for those patients in whom physicians indicated at baseline they would add ezetimibe as opposed to those in whom physicians said the addition was not needed (38.9% vs. 25.9%, p=0.023). This finding was even more significant with respect to the use of PCSK9 (43.3% vs 22.0%, p<0.0001).
Clinical outcomes such as ACS, CVA/TIA, PCI, CABG, or hospitalization for ASCVD reasons were recorded in 10.7% of patients during the follow up. Patients with no event had an overall LDL-C of 1.90 ± 1.3 mmol/L while those with an event had LDL-C significantly higher at the visit immediately prior to event (2.70 ± 1.35, p=0.0001); moreover in patients with an event, the LDL-C level after the event was lower as compared to those without an event at the end of the follow up (1.61 ± 1.02 vs 1.90 ± 1.3, p=0.0002).
Discussion
Patients with ASCVD are at risk for major adverse cardiac events such as death, acute coronary syndromes, and revascularization. While evidence based secondary prevention strategies are recommended to lower the risk of recurrent events, many patients appear not to be managed according to recommendations. Our study was designed to address the care gap in patients with ASCVD with the specific focus on management of dyslipidemia.
In patients with established cardiovascular disease, LDL-C lowering is one of the safest and efficient ways of lowering the risk of future cardiovascular events including cardiovascular and total mortality and myocardial infarction and stroke. Lowering of LDL-C by 1 mmol/L results in 20% reduction in cardiovascular mortality and 12% reduction in total mortality as well as 22% reduction in all cardiovascular events over five years [1]. Thus, a mean reduction of LDL-C of over 1 mmol/L observed in GOAL program, if sustained, has the potential to provide an important reduction of ASCVD related major adverse cardiac events. More than half of high-risk patients could achieve the recommended LDL-C level as a result of physician reminder as an educational intervention.
The significant decrease in LDL was the direct result of additional lipid lowering therapy based on the CPG recommendations [2]. It is important to note that the baseline use of high intensity statin as per recommendations was very high indicating physician willingness to follow the guidelines with respect to all three recommended lipid lowering therapies. Significant increase in the use of additional lipid lowering therapy also confirms the efficacy of educational intervention when delivered as a QI program using patient level data [3,15].
Care gap (difference between recommended and prescribed therapy) is multi-factorial including a number of patient and physician associated factors [16,17] and is associated with unfavourable outcome [18]. Our findings of a significantly higher LDL-C level in patients with ASCVD event immediately before the event indicates physician discounting the risk of an event in a patient with chronic disease who appears to be stable but for elevated LDL-C level. This treatment inertia was the specific target of our educational intervention. Once the event occurred, the physicians saw the need to optimize management and reduce the risk of future event with addition of evidence-based lipid lowering therapies.
The impact of programs like GOAL is significant given the LDL-C reduction demonstrated and expected reduction in cardiovascular events associated with LDL lowering. Thus, clinician-oriented support tools addressing both knowledge and care gap (implementation science) is of value as an extension of professional guidelines and should be considered as an important approach towards quality-of-care improvement.
Limitations
Selection bias at the physician and patient level may limit the generalizability of our findings. The educational intervention was not applied at the time of the clinical encounter itself, i.e. it was possible for physicians to enter the data at some later point. This was the reason for one of the choices being: “I will follow the guidelines and prescribe during the next visit”.
COVID-19 pandemic disrupted, delayed, and reduced the number of patients available for the timely follow up.
Conclusion
The results of GOAL International program indicate the feasibility of delivering an educational intervention and as a result overcoming treatment inertia and improving LDL-C control which should help to achieve reduction in cardiovascular morbidity and mortality of ASCVD patients.
Disclosures
Anatoly Langer received implementation science research grants in the therapeutic area of dyslipidemia from Amgen and Novartis.
Marco Alcocer-Gamba received research grants with Amgen, AstraZeneca, Bayer, Pfizer, Sanofi, Servier.
Otavio Berwanger received Research grants from AstraZeneca, Pfizer, Bayer, Amgen, Servier, BMS, and Novartis.
Wael Almahmeed and Khalid Al Faraidy declare that there are no conflicts of interest regarding the publication of this article.
Funding Statement
Study was supported by Amgen. The funding organization did not participate in study design, data collection, data analysis, manuscript preparation and/or publication decisions; all of which were decided upon by the lead author in consultation with the steering committee.
Statement of Author Contribution
- Anatoly Langer: Overall study design, site and data coordination, analyses, and lead author.
- Mousa Akbar: study design, country specific approach for site selection and patient enrolment, data interpretation, drafting article, data collection.
- Marco Alcocer Gamba: study design, country specific approach for site selection and patient enrolment, data interpretation, drafting article, data collection.
- Wael Almahmeed: study design, country specific approach for site selection and patient enrolment, data interpretation, drafting article, data collection.
- Khalid Al Faraidy: study design, country specific approach for site selection and patient enrolment, data interpretation, drafting article, data collection.
- Otavio Berwanger: study design, country specific approach for site selection and patient enrolment, data interpretation, drafting article, data collection.
- Mary Tan: statistics.
- Caroline Spindler: study coordination and enrolment, query resolution, participating site support.
- Diane Camara: study coordination and enrolment, query resolution, participating site support.
References
2. Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al. 2019 ESC/EAS Guidelines for the management of dyslipidemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2020 Jan;41(1):111-88.
3. Langer A, Tan M, Goodman SG, Grégoire J, Lin PJ, Mancini GBJ, et al. GOAL Canada: Physician education and support can improve patient management. CJC Open. 2019 Dec;2(2):49-54.
4. Grima DT, Leiter LA, Goodman SG, Attard CL, Chow C-M, Langer A. How many cardiovascular events can be prevented with optimal management of high-risk Canadians? Can J Cardiol. 2008 May;24(5):363-8.
5. Pearson GJ, Thanassoulis G, Anderson TA, Barry AR, Couture P, Dayan N, et al. 2021 CCS Guidelines for the Management of Dyslipidemia for the Prevention of Cardiovascular Disease in the Adult. Can J Cardiol. 2021 Aug;37(8):1129-50.
6. Grundy SM, Stone NJ, Bailey AL Beam C, Birtcher KK, Blumenthal RS, et al. AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines". J Am Coll Cardiol. 2019;73:e285-e350.
7. Martineau P, Gaw A, de Teresa E, Farsang C, Gensini GF, Leiter LA, et al. Effect of individualizing starting doses of a statin according to baseline LDL-cholesterol levels on achieving cholesterol targets: the Achieve Cholesterol Targets Fast with Atorvastatin Stratified Titration (ACTFAST) study. Atherosclerosis. 2007 Mar;191(1):135-46.
8. Wiviott SD, Cannon CP, Morrow DA, Ray KK, Pfeffer MA, Braunwald E, et al. Can low-density lipoprotein be too low? The safety and efficacy of achieving very low low-density lipoprotein with intensive statin therapy: A PROVE IT-TIMI 22 Substudy. J Am Coll Cardiol. 2005 Oct;46(8):1411-6.
9. Cannon CP, Blazing MA, Giugliano RP, McCagg A, White JA, Theroux P, et al. Ezetimibe added to statin therapy after acute coronary syndromes. N Engl J Med. 2015 Jun;372(25):2387-97.
10. Sabatine MS, Giugliano RP, Keech AC, Honarpour N, Wiviott SD, Murphy SA, et al. Evolocumab and clinical outcomes in patients with cardiovascular disease. N Engl J Med. 2017 May;376(18):1713-22.
11. Schwartz GG, Szarek M, Bhatt DL et al. The ODYSSEY OUTCOMES Trial: Topline Results. Alirocumab in patients after acute coronary syndrome. Presented at the American College of Cardiology Annual Scientific Sessions March 10, 2018.
12. Langer A, Tan M, Bell A, Ngui D, Mah D, Mehan U, et al. Can Physician Education and Support Improve Patient Management. Cardiol Vasc Res. 2020;4:1-5.
13. Sud M, Han L, Koh M, Abdel-Qadir H, Austin PC, Farkouh ME, et al. Low-density lipoprotein cholesterol and adverse cardiovascular events after percutaneous coronary intervention. J AM Coll Cardiol. 2020 Sept;76(12):1440-50.
14. Nelson AJ, Haynes K, Shambhu S, Eapen Z, Cziraky MJ, Nanna MG, et al. High-intensity statin use among patients with atherosclerosis in the U.S. J Am Coll Cardiol. 2022 May;79(18):1802-13.
15. Langer A, Tan M, Cieza T, Ciomyk R, Graham J, Ramanathan K, et al. Can clinical reminder help optimize the use of secondary prevention therapies in non-ST elevation acute coronary syndrome? Int J Cardiol Cardiovasc Med. 2018 Jan;1(1):1-5.
16. Rapezzi C, Biagini E, Bellis P, Cafiero M, Velussi M, Ceriello C, et al. Exploring the gap between National Cholesterol Education Program guidelines and clinical practice in secondary care: results of a cross-sectional study involving over 10 000 patients followed in different specialty settings across Italy. J Cardiovasc Med. 2008 Sep;9(9):878-87.
17. Tsang JLY, Mendelsohn A, Tan MKK, Hackam DG, Leiter LA, Fitchett D, et al. Discordance between physicians' estimation of patient cardiovascular risk and use of evidence-based medical therapy. Am J Cardiol. 2008 Nov;102(9):1142-5.
18. Rogers AM, Ramanath VS, Grzybowski M, Riba AL, Jani SM, Mehta R, et al. The association between guideline-based treatment instructions at the point of discharge and lower 1-year mortality in Medicare patients after acute myocardial infarction: the American College of Cardiology's Guidelines Applied in Practice (GAP) initiative in Michigan. Am Heart J. 2007 Sep;154(3):461-9.
