Abstract
Introduction: Hypertension (HTN) is a major public health issue and is both a cause and a common complication of chronic kidney disease (CKD). This study aimed to determine the prevalence of HTN and identify its associated factors in patients with advanced CKD in Parakou, Benin.
Patients and Methods: A cross-sectional study was conducted in the Nephrology Department of the CHUD-B/A hospital from April 01, 2023, to August 31, 2023. We included all consenting patients aged 15 and over with stage 3 to 5 CKD. The presence of HTN was the main outcome variable. A descriptive and comparative analysis was performed, using Chi-square or Fisher's exact test to identify associated factors. A p-value <0.05 was considered significant.
Results: A total of 72 patients were included. HTN was highly prevalent in this cohort, affecting 86.1% (62 out of 72 patients). Bivariate analysis revealed a significant association between HTN and lower limb edema (p=0.004; OR=8.82) and advanced stage of CKD (p=0.02; OR=4.86). Due to the very small size of the non-hypertensive group (n=10), multivariate logistic regression could not be performed.
Conclusion: HTN was exceedingly high among patients with advanced CKD in our cohort (86.1%). The strong, unadjusted association with clinical signs of volume overload underscores the importance of fluid management in addition to antihypertensive therapy in these patients.
Keywords
Hypertension, Chronic kidney disease, Associated factors, Parakou, Benin
Introduction
High blood pressure (BP) is a major public health problem. According to the World Health Organization (WHO), 1 billion 28 million people worldwide aged 30-79 years are hypertensive, and most of them (two-thirds) live in low- and middle-income countries [1]. It is the main risk factor for heart disease, stroke and kidney failure [2]. Chronic kidney disease (CKD) is another common and growing problem. In 2015, more than 353 million people, or 5% of the world's population, suffered from CKD [3]. In the United States, the estimated prevalence of all stages of CKD is approximately 13%, and this disease affects nearly 20 million Americans [3].
There is a correlation between renal failure and hypertension (HTN), which is complex [4]. Indeed, HTN is both a cause and a complication of renal failure [2]. On the one hand, HBP is a potential cause of chronic renal failure, as it is responsible for approximately 30% of cases of end-stage renal disease (ESRD) [4]. On the other hand, it is a frequent consequence of chronic renal failure: 80% of patients suffering from chronic renal failure have high BP at some point during the course of their kidney disease [4]. The occurrence of HTN increases as renal function is impaired. Other factors, such as age, the presence of proteinuria and underlying renal disease, also determine the prevalence of HTN in CKD patients [5].
In Europe, in 2012, in the CREDIT study (Chronic Renal Disease In Turkey) on chronic kidney disease in Turkey, the prevalence of HTN among CKD patients was 56.3%, which increased to 84.9% when only CKD was considered. It increased with increasing stage of CKD, from 79.8% at the moderate CKD stage to 92.3% at the ESRD stage [6].
In Africa, particularly in Mali, in 2019, a study on HTA during CKD reported a prevalence of 100% in chronic kidney failure patients. Women were more prone to this comorbidity, as were patients with pathological proteinuria. Similarly, hypertriglyceridemia is found in almost half of the patients [7].
In Benin, particularly at the Borgou/Alibori Departmental University Hospital (CHUD B/A), HTN was found in 68.85% of patients with chronic renal failure according to a study conducted in the Internal Medicine department of the said hospital in 2019 [8]. The frequent existence of HTN-IRC comorbidity and the importance of knowing the complications inherent to this comorbidity justify the present work, the objective of which was to study the factors associated with high BP in patients with CKD at CHUD B/A in 2023.
Patients and Methods
Study design and setting
A cross-sectional study was conducted in the Nephrology Department of the Borgou and Alibori Departmental Teaching Hospital (CHUD-B/A) in Parakou, Benin. The study took place over a five-month period, from April 01, 2023, to August 31, 2023.
Study population and sampling
This study included all patients diagnosed with stage 3, 4, or 5 CKD who were followed in the department during the study period. A consecutive sampling approach was applied, enrolling every patient who met the predefined eligibility criteria. To be included, participants had to be aged 15 years or older, have a confirmed diagnosis of CKD at stages 3, 4, or 5, and possess the capacity to answer study-related questions. Informed consent was obtained from all eligible participants. Patients whose laboratory data required for analysis were incomplete were excluded from the study.
Variables and definitions
The dependent variable was the presence of HTN. Patients were considered hypertensive if they met at least one of the following criteria:
- A prior diagnosis of HTN and currently on antihypertensive medication, regardless of the current BP reading.
- A measured systolic blood pressure ≥140 mmHg and/or a diastolic blood pressure ≥90 mmHg.
CKD was defined as a glomerular filtration rate (GFR) below 60 ml/min/1.73m² for at least three months.
The independent variables included sociodemographic characteristics, behavioral factors, clinical findings, laboratory results, and therapeutic data.
Data collection
Data were collected through structured one-on-one interviews with patients using a semi-structured questionnaire. This questionnaire was designed on the KoBoToolbox platform and administered digitally via the KoboCollect application (Version 1.30.1) on a smartphone.
BP was measured with a Spengler Tensonic electronic tensiometer. Measurements were taken on the right arm after the patient had been seated and at rest for 15 minutes. Three separate readings were taken at 5-minute intervals, and the average of the last two readings was recorded as the patient's official BP.
Statistical analysis
Once collected, the data was exported from the KoBoToolbox server to an Excel file. Only complete records were retained, and patients with incomplete laboratory data required for analysis were excluded to prevent bias associated with missing data. Statistical analysis was performed using EpiInfo (version 7.2.3.1) and STATA 12 software.
Descriptive statistics were used to summarize the data. Quantitative variables were presented as means with their standard deviations (SD), while qualitative variables were presented as frequencies and proportions.
For comparative analysis, patients were divided into two groups: hypertensive and non-hypertensive. To identify factors associated with HTN, the characteristics of these two groups were compared using the Chi-square (χ²) test or Fisher's exact test for categorical variables, with the latter being used for small sample sizes. A p-value of less than 0.05 was considered statistically significant. Due to the very small size of the non-hypertensive group (n=10), we were unable to perform multivariate logistic regression. Therefore, all associations reported are unadjusted and bivariate only.
Ethical considerations
This study was conducted as part of a research project at the Faculty of Medicine of the University of Parakou. Informed consent was obtained from the participants or their legal guardians. Rules of anonymity and confidentiality of information were respected.
Results
Participation flow and characteristics
A total of 72 patients were included. The prevalence of HTN was 86.1% (62 out of 72 patients). Males accounted for 66.1%, with a sex ratio of 1.9.
Table 1 presents the comparative baseline characteristics of the study population, categorized by hypertension status. The mean age of the overall cohort was 54.3±14.7 years.
|
|
Total (N=72) |
Hypertensive Group (n=62) |
Non-Hypertensive Group (n=10) |
p-value |
|
I. Demographic data |
||||
|
Mean age (years), mean ± SD |
54.3±14.7 |
52.7±14.4 |
≈64.3±10.4 |
0.68 |
|
Male gender, n (%) |
54 (75.0%) |
47 (75.8) |
7 (70.0) |
0.73 |
|
II. Comorbidities and risk factors |
||||
|
Diabetes mellitus, n (%) |
16 (22.2%) |
14 (22.6) |
2 (20.0) |
1.00 |
|
Primary education level (or less), n (%) |
31.9 |
22 (35.5) |
1 (10.0) |
<0.001 |
|
Regular tobacco exposure, n (%) |
16 (22.2%) |
14 (22.6) |
2 (20.0) |
1.00 |
|
III. Clinical and evolutionary parameters |
||||
|
Vascular nephropathy (etiology), n (%) |
51 (70.8%) |
51 (82.3) |
0 (0.0) |
0.001 |
|
Severe/end-stage CKD (stage 4 or 5), n (%) |
63.8 |
43 (69.4) |
3 (30.0) |
0.02 |
|
Pelvic limb edema (PLE), n (%) |
29 (40.3%) |
29 (46.8) |
0 (0.0) |
0.004 |
|
IV. Biochemical parameters (mean ± SD) |
|
|
|
|
|
Serum urea (g/l) |
1.97±1.32 |
1.98±1.33 |
1.90±1.26 |
0,83 |
|
Serum creatinine (mg/l) |
11.9±6.1 |
11.9±6.1 |
11.9±6.0 |
1.00 |
Advanced CKD
Among hypertensive patients, 74.2% had suffered from advanced CKD for less than one year, and 3.2% had suffered from it for more than 3 years.
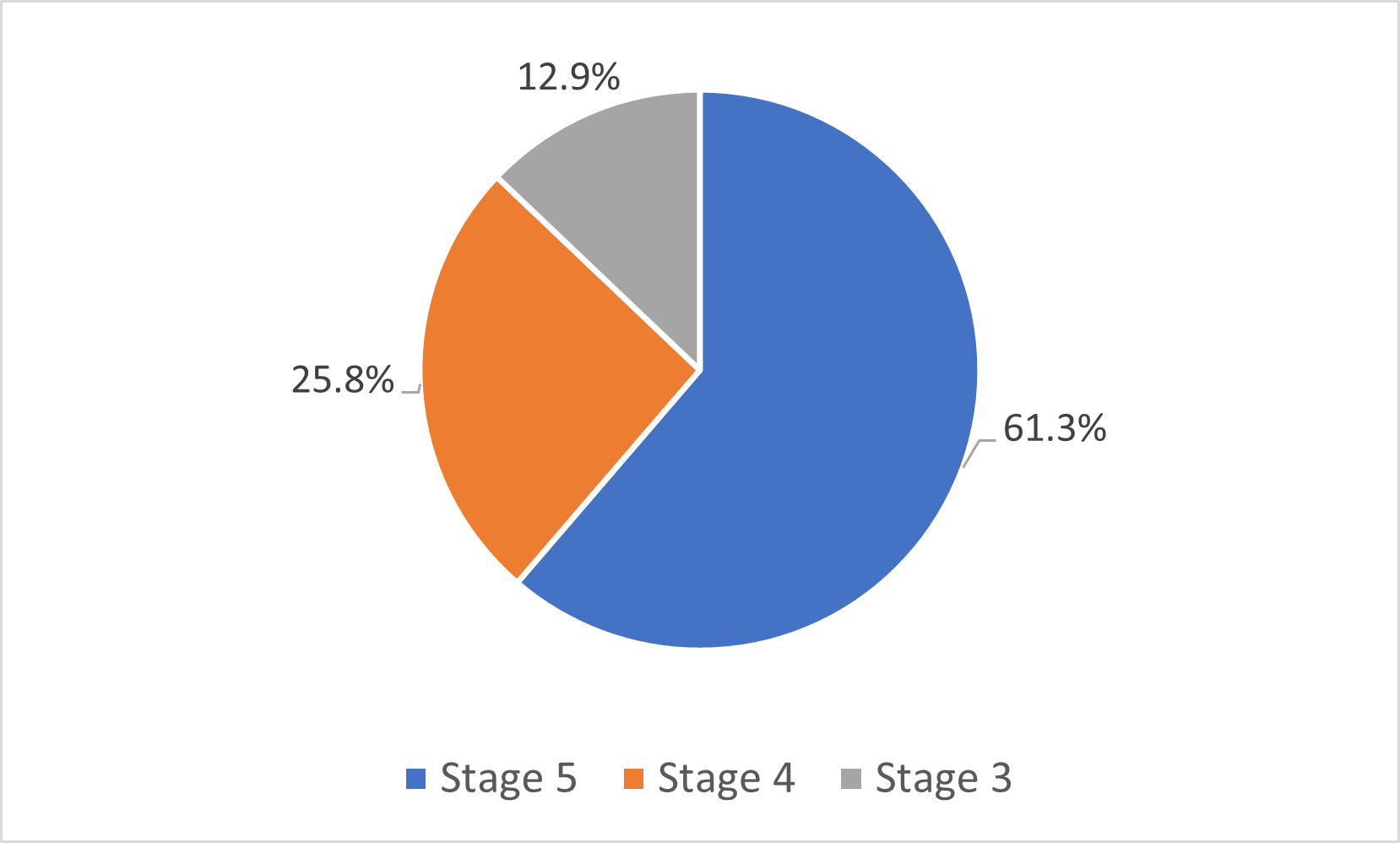
Stages 3, 4 and 5 CKD were found in 12.9%, 25.8%, and 61.3% of the patients, respectively (Figure 1).
Figure 1. Distribution of hypertensive patients in the Nephrology Department of CHUD-B/A according to the stages of chronic kidney disease (n=62).
Anatomo-clinical diagnosis of advanced CKD
Among the 62 patients, 82.3% had chronic vascular nephropathy, 9.7% had chronic glomerular nephropathy, and 6.5% had chronic interstitial nephropathy.
Prevalence of high BP in patients with CKD
Among the 72 patients with advanced CKD, 62 were hypertensive, with a prevalence of 86.1%.
High BP grades
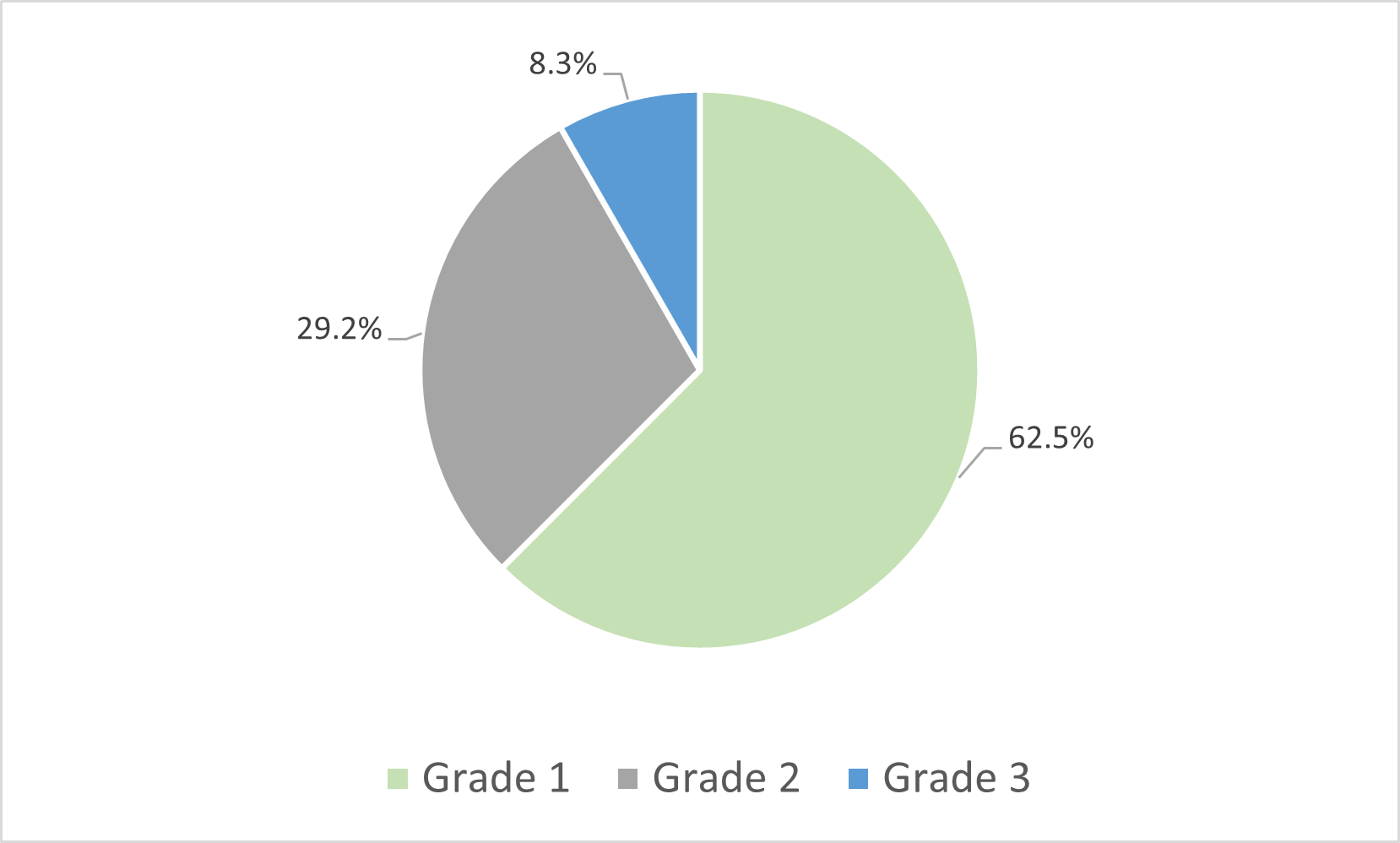
Grades 1, 2, and 3 HTN were found in 62.5%, 29.2%, and 8.3% of the patients, respectively (Figure 2).
Figure 2. Distribution of hypertensive patients suffering from chronic kidney disease in the Nephrology Department of CHUD-B/A according to the grade of arterial hypertension (n=62).
Types of high BP
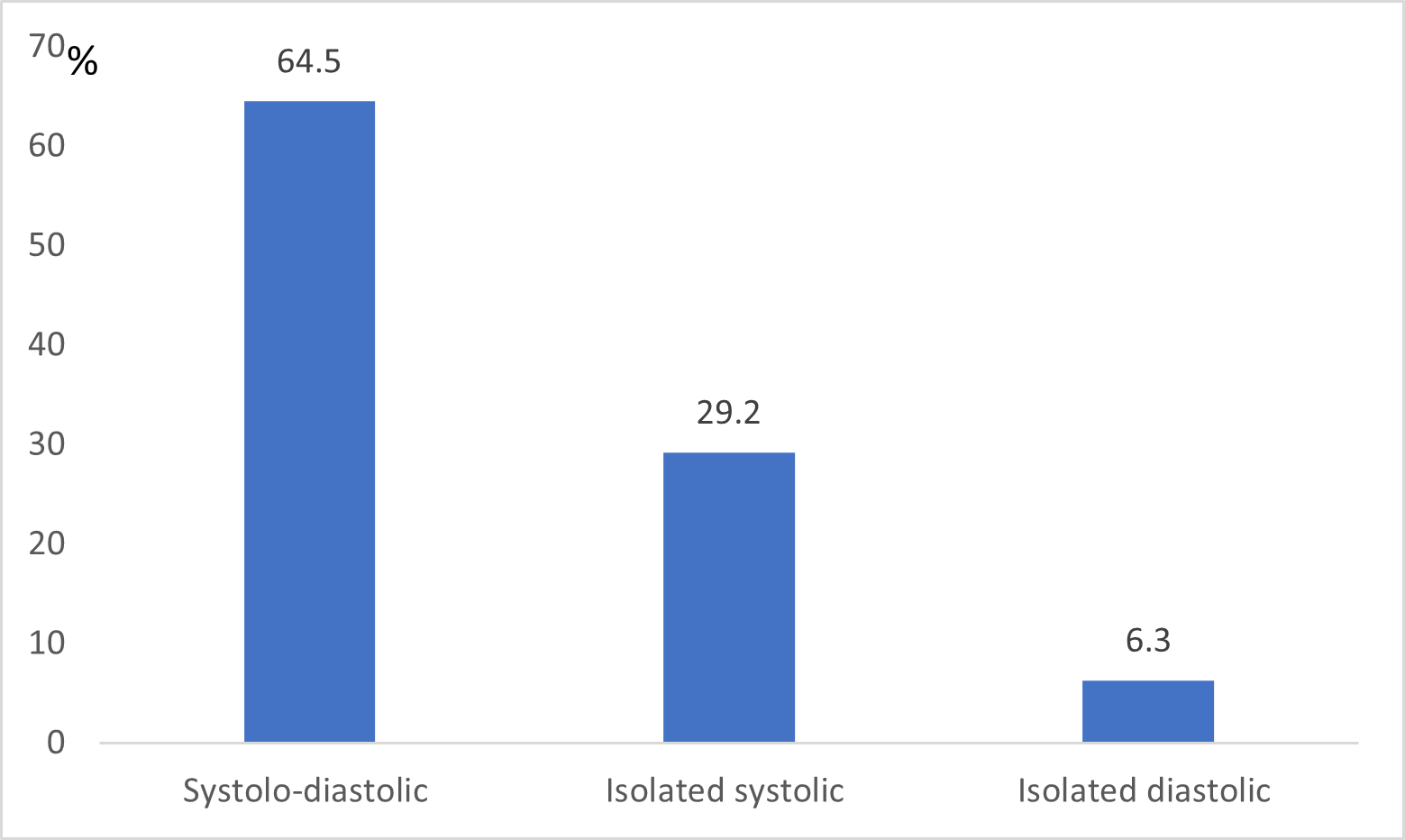
Systolic–diastolic HTN was the most common HTN (64.5%), followed by isolated systolic HTN (29.2%) and isolated diastolic HTN (6.3%) (Figure 3).
Figure 3. Distribution of hypertensive patients suffering from chronic kidney disease in the Nephrology Department of CHUD-B/A according to the type of arterial hypertension (n=62).
Clinical aspects
Among the 62 patients, 65.4% reported asthenia, 38.2% reported lower limb edema, 29.1% reported dyspnea, 21.8% reported headache, 16.4% reported abdominal pain, 12.7% reported anorexia, 10.9% reported visual disturbance, 9.1% reported nausea and vomiting, 9.1% reported dizziness, 3.4% reported anuria, and 1.8% reported ringing in the ears.
A total of 82.3% and 22.6% of the known hypertensive patients were under treatment or not and diabetic and victims of vascular and cerebral accidents, respectively. Among the patients surveyed, 14 (22.6%) were regularly exposed to tobacco, 23 (37.1%) regularly consumed alcohol, 1 (17.7%) did not regularly consume fruits and vegetables, 40 (64.5%) consumed overly salty meals, and 58 (93.5%) did not perform physical activity. On physical examination, 21 patients (33.9%) had conjunctival pallor, 61 patients (98.4%) had a normal respiratory rate, 42 patients (67.7%) had a heart rate, and 29 patients (46.8%) had lower limb edema.
The urine dipstick revealed albuminuria with one cross, two crosses and at least three crosses in 22.2%, 22.2% and 33.3% of patients, respectively. Leukocyturia and hemoglobinuria were found in 27.7% and 33.3%, respectively.
Among the 62 patients, 27.4% had signs of right heart failure, 14.5% had signs of left heart failure, 21.0% had hepatomegaly, and 17.7% had ascites.
Paraclinical data
Among the 62 patients, 98.4% had hyperuricemia, 29.0% had hyponatremia, 1.6% had hypernatremia, 14.5% had hypokalemia, 16.1% had hyperkalemia, 54.4% had hypocalcemia, 23.4% had total hypercholesterolemia, 100% had HDL hypercholesterolemia, 17.8% had hypertriglyceridemia, and 61.1% had hyperphosphatemia. Among the 62 patients, 46 (74.2%) had dedifferentiated, atrophied, and hyperechoic kidneys.
Therapeutic profile of hypertensive patients
Among the 62 hypertensive patients, the most prescribed class of antihypertensive medication was calcium channel blockers (91.9%), followed by angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers (ARBs) (56.5%), and diuretics (33.9%).
Factors associated with high BP
To identify factors associated with HTN, a comparative analysis was conducted between the hypertensive (n=62) and non-hypertensive (n=10) groups using Fisher's exact test.
The analysis revealed that the presence of lower limb edema and an advanced stage of CKD were significantly associated with HTN (Table 2).
|
|
Hypertensive (n=62) |
Non-Hypertensive (n=10) |
OR (IC 95 %) |
p-value |
|
Lower Limb Edema |
||||
|
Present, n (%) |
29 (46.8) |
0 (0.0) |
8.82 (1.70−45.71) |
0.004 |
|
Absent, n (%) |
33 (53.2) |
10 (100.0) |
1 |
|
|
CKD Stage |
||||
|
Stage 3 |
8 (12.9) |
4 (40.0) |
1 |
0.02 |
|
Stage 4 & 5 |
54 (87.1) |
6 (60.0) |
4.86 (1.11−21.30) |
|
Discussion
This study investigated the factors associated with HTN among patients with advanced CKD in a tertiary care setting in Benin. The results confirm that HTN is nearly universal in this population, with a prevalence of 86.1%. Our comparative analysis identified lower limb edema and advanced CKD stage as the key factors significantly associated with the presence of hypertension.
Sociodemographic characteristics
The patients in our study had a mean age of 54.3±14.7 years. This average is close to that reported by several authors in Africa, such as Ackoundou N'Guessan et al. in Ivory Coast [10], Ramilitiana et al. in Madagascar [3], and Ngoie et al. in Congo [11], who reported 48.2±14.6 years, 47.0±17.5 years, and 51.4±13.5 years, respectively. The most represented age group in our study was 55–75 years, which is close to that reported in a previous study in Benin (60–70 years) [8] but different from that reported (20–40 years) by Djiguiba in Mali [12].
The average age of the population of patients with chronic renal failure and HTN was 52.7±14.4 years. These same results were reported by Tia et al. in Ivory Coast [13], who reported an average age of 52.6±9 years.
Our series revealed a clear male predominance, with a sex ratio of 1.9. This observation is reproduced by several authors, such as Tia et al. [13]. in the Ivory Coast, Hamadoun et al. [14], in Mali and Madagascar, and Lemrabott et al. in Senegal [15], who reported sex ratios of 1.46, 2.5, and 1.34, respectively. This observation could be explained by the male predominance of chronic renal failure patients [16,17].
Lifestyle
In the population of chronic renal failure and hypertensive patients, 22.6% of patients were regularly exposed to tobacco, which is close to the 26.4% and 18.8% reported by Ngoie et al. [11], in the Congo and by Ahoui et al. [8], in Benin.
Alcohol abuse was reported in 37.1% of the hypertensive patients in our study. This result is higher than that of 20.8% reported by Chaiben et al. [18], in Brazil and significantly lower than that of 64.7% reported by Ngoie et al. [11], in the Congo.
A lack of physical activity was found in 93.5% of the hypertensive patients in our study. This finding is consistent with that of Ahoui et al. [8], and Benin and Ngoie et al. [11], who reported that 65.5% and 71.6%, respectively, of the population in the Congo.
Overall, Beninese patients, like those in other countries, develop the same lifestyle practices.
CKD
In the population of chronic renal failure and hypertensive patients, the most common stage is the terminal stage, followed by the severe stage and then the moderate stage, with proportions of 61.3%, 25.8%, and 12.9%, respectively. Sinomono et al. in the Democratic Republic of the Congo [19] reported similar proportions for the terminal, severe, and moderate stages, which were 72.5%, 16.7%, and 5.1%, respectively. Patients received nephrologic treatment at an advanced stage. Renal disease is also silent, and it is only at the advanced stage that most signs appear.
In hypertensive patients in our study, the most common chronic renal lesion was chronic vascular nephropathy in 82.3% of patients, followed by chronic glomerular nephropathy in 9.7% of patients and tubulointerstitial nephropathy in 6.5% of patients. Sinomono et al. in the Democratic Republic of the Congo [19] reported that chronic glomerulonephritis was the primary cause, accounting for 38.8%, followed by nephroangiosclerosis, accounting for 21.8%, and tubulointerstitial nephropathy, accounting for 15.5%. The marked dominance of chronic vascular nephropathy (82.3%) in our cohort, compared to the higher prevalence of chronic glomerulonephritis reported in other African studies, is likely a reflection of our study population being patients with pre-existing, advanced CKD. Since uncontrolled hypertension is a major cause of vascular nephropathy and given the high prevalence of HTN in our region, it is plausible that a significant proportion of these advanced cases represent established hypertensive nephrosclerosis. Furthermore, the bidirectional relationship between HTN and CKD means that HTN, as both a cause and a consequence, may have obscured or progressed from other initial etiologies, making vascular damage the dominant and late-stage presentation.
Prevalence of high BP in patients with chronic kidney failure
The prevalence of HTN was 86.1%, comparable to that reported in studies by Argawal et al. in the United States [20], Babua et al. in Uganda [21] and Djiré [7] in Mali, with 86%, 90%, and 91.2%, respectively. On the other hand, Altun et al. in Turkey in 2012 [6] and Djiguiba in Mali [12] reported that the prevalence of hypertension was lower than that reported in our study, i.e., 56.3% and 33.4%, respectively. This difference could be explained by the larger size of our sample.
Factors associated with high BP in patients with chronic kidney failure
This study highlights a significant association between lower limb edema and HTN (p=0.004; OR=8.82) in patients with CKD, suggesting that edema may serve as a clinical marker of volume-dependent HTN. The findings aligned with recent literature showing that impaired renal sodium and water excretion leads to extracellular fluid expansion and hypervolemia, which in turn contributes to elevated BP. Supporting evidence from Roşu et al. (2025) and Kilaparthi et al. (2025) confirms that peripheral edema is frequently observed in hypertensive CKD patients, especially in advanced stages or glomerular pathologies. These results underscore the importance of incorporating volume status assessment in the management of HTN in CKD and advocate for a therapeutic approach that addresses both fluid overload and BP control [22,23].
This study confirms a significant association between advancing stages of CKD and the severity of HTN (p=0.02; OR=4.86), supporting the theory that as renal function declines, the kidneys' ability to excrete sodium and water diminishes, leading to volume overload. The resulting hypervolemia contributes directly to volume-dependent HTN, particularly in CKD stages 4 and 5. Recent literature, including work by Nagata and Hishida (2024), describes this as a vicious cycle where hypertension exacerbates renal injury, and vice versa. Similarly, Massy and Drueke (2025) emphasize that patients with advanced CKD exhibit increased vascular stiffness and sodium retention, contributing to more resistant hypertension. These findings underscore the importance of volume control and individualized BP management strategies in patients with moderate-to-severe CKD [24,25]. However, due to the unadjusted nature of these findings, the independent role of HTN stage as a predictor of advanced CKD in this specific cohort cannot be definitively established without multivariate control for confounding factors. In patients with advanced CKD and concomitant HTN, the coexistence of inflammatory conditions adds further complexity to clinical care. Ensuring access to safe and effective therapeutic options remains a major priority. Notably, recent real-world evidence from Türkiye demonstrated that biologic DMARDs (disease-modifying antirheumatic drugs) could be used safely and effectively in spondyloarthritis patients with CKD, underscoring the importance of carefully maintaining comprehensive management of comorbidities in this high-risk population [26].
Strengths and limitations
A key strength of this study is its use of clear, standardized definitions for both CKD and HTN, which allows for meaningful comparisons with other research.
However, the study has several important limitations. First, its cross-sectional design does not allow for the determination of causality; it is impossible to know whether HTN was the cause or the consequence of CKD in these patients, as the relationship is famously bidirectional. Second, the very small size of the non-hypertensive group (n=10) prevented us from performing a multivariate logistic regression. This is a major methodological limitation, as we could not adjust for potential confounding variables (like age, diabetes, or lifestyle factors) to identify independent predictors. The associations we report are therefore unadjusted and prone to confounding bias. This underscores the urgent need for larger, multicenter studies across Benin and West Africa to gather a more representative and diverse non-hypertensive CKD cohort, which is essential for establishing robust, independent risk factors in this population.
Conclusion
Hypertension is common in patients with chronic kidney failure, with significant prevalence. There were multiple associated factors. Control of hypertension in patients with chronic kidney failure should involve therapeutic education and adherence to hygiene and dietary measures.
References
2. Hamrahian SM, Falkner B. Hypertension in Chronic Kidney Disease. Adv Exp Med Biol. 2017;956:307–25.
3. Ramilitiana B, Ranivoharisoa EM, Dodo M, Razafimandimby E, Randriamarotia WF. Une étude rétrospective sur l'incidence de l'insuffisance rénale chronique dans le service de Médecine Interne et Néphrologie du Centre Hospitalier Universitaire d'Antananarivo [A retrospective study on the incidence of chronic renal failure in the Department of Internal Medicine and Nephrology at University Hospital of Antananarivo (the capital city of Madagascar)]. Pan Afr Med J. 2016 Mar 28;23:141. French.
4. Pruijm M, Battegay E, Burnier M. Arterial hypertension and renal failure. Forum Med Suisse. 2009;9(28-29):497–501.
5. Andersen MJ, Agarwal R. Etiology and management of hypertension in chronic kidney disease. Med Clin North Am. 2005 May;89(3):525–47.
6. Altun B, Süleymanlar G, Utaş C, Arınsoy T, Ateş K, Ecder T, et al. Prevalence, awareness, treatment and control of hypertension in adults with chronic kidney disease in Turkey: results from the CREDIT study. Kidney Blood Press Res. 2012;36(1):36–46.
7. Djiré P. Arterial hypertension in chronic kidney disease [thèse Internet]. Bamako (Mali): USTTB; 2020. Disponible à: https://library.adhl.africa/handle/123456789/13713.
8. Ahoui S, Dovonou CA, Vigan J, Agboton BL, Alassani CA, Doritchamou E, et al. Frequency and factors associated with chronic renal failure in the Internal Medicine Department of the Borgou Departmental University Hospital. Afr J Intern Med. 2021;8:8-16.
9. Fourcade L, Paule P, Mafart B. Hypertension artérielle en Afrique subsaharienne actualité et perspectives [Arterial hypertension in sub-Saharan Africa. Update and perspectives]. Med Trop (Mars). 2007 Dec;67(6):559–67. French.
10. Ackoundou-N'Guessan KC, N'Zoue S, Lagou AD, Tia MW, Guei CM, Coulibaly AP, et al. Épidémiologie de l'hypertension artérielle non contrôlée au cours des maladies rénales chroniques chez des patients admis dans une unité de néphrologie d'Afrique noire : une étude rétrospective de 479 patients [Uncontrolled hypertension in chronic kidney disease in patients from black Africa admitted in a renal unit: a retrospective analysis]. Nephrol Ther. 2014 Dec;10(7):518–27. French.
11. Ngoie SM, Mulenga P, Mukuku O, Kakisingi CN, Sangwa CM, Nawej PT, et al. Maladie rénale chronique: facteurs associés, étiologies, caractéristiques clinique et biologique à Lubumbashi en République Démocratique du Congo [Chronic kidney disease: associated factors, etiologies, clinical and biological parameters at Lubumbashi city in Democratic Republic of Congo]. Pan Afr Med J. 2017 Sep 15; 28:41. French.
12. Djiguiba K. The prevalence of high blood pressure in HIV-positive chronic kidney failure patients in the Nephrology and Hemodialysis Department of Point G [thèse Internet]. Bamako (Mali): University of Bamako; 2007 [cité 21 oct 2023]. Disponible à: https://www.bibliosante.ml/handle/123456789/8047.
13. Tia MW, Nda JK, Kouame GR, Kobenan R, Daingui D, Ouattara B. Chronic renal failure: epidemiological, diagnostic, therapeutic and evolutionary aspects at the Bouaké University Hospital from 2016 to 2020. Afr J Intern Med. 2022;9(2-2):60-66. Disponible à: http://www.rafmi.org/index.php/rafmi/article/view/5656.
14. Hamadoun Y, Samaké M, Fofana AS, Simaga S, Touré A, Coulibaly N, et al. Prévalence et Complications de l’Hypertension Artérielle Maligne dans le Service de Néphrologie du CHU du Point G. HEALTH SCIENCES AND DISEASE. 2020 Mar 21;21(4).
15. Lemrabott A, Keita IA, Faye M, Fall K, Cissé MM, Mbengue M, Niang A, Diouf B, Ka EH. Hypertension artérielle secondaire aux glomérulopathies chroniques primitives au Sénégal. Néphrologie & Thérapeutique. 2018 Sep 1;14(5):345.
16. Stengel B, Couchoud C, Helmer C, Loos-Ayav C, Kessler M. Epidémiologie de l'insuffisance rénale chronique en France [Epidemiology of chronic kidney disease in France]. Presse Med. 2007 Dec;36(12 Pt 2):1811–21. French.
17. University College of Nephrology Teachers. Chronic renal failure and chronic kidney disease. In: Nephrology Course. 8th ed. Paris: Ellipses; 2018. p. 26.
18. Chaiben VBO, Silveira TBD, Guedes MH, Fernandes JPA, Ferreira JHF, Beltrão J, et al. Cognition and renal function: findings from a Brazilian population. J Bras Nefrol. 2019 Apr-Jun;41(2):200–07.
19. Eyeni Sinomono DT, Loumingou R, Gassongo Koumou GC, Mahoungou GH, Mobengo JL. Chronic renal failure in the brazzaville university hospital center: Epidemiological, clinical and evolutionary aspects. Saudi J Kidney Dis Transpl. 2021 Sep-Oct;32(5):1450–5.
20. Agarwal R, Nissenson AR, Batlle D, Coyne DW, Trout JR, Warnock DG. Prevalence, treatment, and control of hypertension in chronic hemodialysis patients in the United States. Am J Med. 2003 Sep;115(4):291–7.
21. Babua C, Kalyesubula R, Okello E, Kakande B, Sebatta E, Mungoma M, et al. Cardiovascular risk factors among patients with chronic kidney disease attending a tertiary hospital in Uganda. Cardiovasc J Afr. 2015 Jul-Aug;26(4):177–80.
22. Roşu CD, Bolintineanu SL, Căpăstraru BF, Iacob R, Stoicescu ER, Petrea CE. Risk factor analysis in vascular access complications for hemodialysis patients. Diagnostics. 2025 Jan 2;15(1):88
23. Kilaparthi Y, Jali S, Jena A. WCN25-2572 C3 Glomerulonephritis–A Rare Cause OF Acute Glomerulonephritis In A Young Male With HBH Disease. Kidney International Reports. 2025 Feb 1;10(2):S212.
24. Nagata D, Hishida E. Elucidating the complex interplay between chronic kidney disease and hypertension. Hypertension Research. 2024 Dec;47(12):3409-22.
25. Massy ZA, Drueke TB. Cardiovascular disease in patients with chronic kidney disease: arteriosclerosis vs. atherosclerosis. European Journal of Preventive Cardiology. 2025 Feb 28:zwaf108.
26. Bulut Gökten D, Tezcan ME, Yağız B, Erden A, Kimyon G, Yaşar Bilge NŞ, et al. Real-World Insights From Türkiye: Biologic DMARDs Usage in Spondyloarthritis Patients With Chronic Kidney Disease. Int J Rheum Dis. 2025 May;28(5):e70274.