Abstract
B-acute lymphoblastic leukemia (B-ALL) often grants with pancytopenia or bicytopenia, with thrombocytopenia being the most important parameter. The case of a 2-year-old child presented as a limp with bicytopenia on peripheral smear was presented. On bone marrow examination, 75% morphologically lymphoid blasts, block positive for periodic-acid Schiff on cytochemistry were found. The blasts suppressed the erythroid population but not the megakaryocytic population. On flow cytometry, a diagnosis was made as common-ALL-antigen positive B-precursor ALL. To conclude, a bone marrow aspirate is decisive in patients with bi/pancytopenia who present with a normal platelet count.
Keywords
B-cell acute lymphocytic leukemia, Normal platelet count, Bicytopenia, Limping, Bone marrow biopsy
Introduction
Limping in children is a common complaint made at pediatric, pediatric orthopedic and in emergency departments [1-3]. It is defined as a deviation from the normal gait pattern expected for the child’s age [4]. Especially in young children, the ambiguities in the signs and symptoms necessitate extensive investigations to enable a reliable medical assessment for the etiological dilemma of limping.
B-acute lymphoblastic leukemia (B-ALL) is a neoplasm of precursor cells, in the B-cell lineage, involving bone marrow and blood. B-ALL mostly presents with bone marrow failure in the form of fatigue, lethargy, persistent fever, bruising or bleeding, and bone and joint pain [5]. Eventhough, ALL is the most common childhood malignancy accounting for 20% of all carcinoma and 70% of all leukemia diagnosed among patients younger than 20 years of age [5], its’ presentation with normal platelet count is rare.
In this sense, acute leukemia (AL) can be answerable for limping, sometimes manifesting as the initial symptom of the disease. Therefore, we believe it is useful to garner our experience to review a clinical presentation of B-ALL diagnosed following a pediatric consultation for limping with a normal platelet count.
Case Presentation
History
A 2-year-old developmentally normal child was brought to the accident and emergency department for the first time for protective limping attributed by his parents to a fall from a height the day before. The pain seemed to involve both the right knee joint and thigh, without precise localization.
He was the 2nd child of non-consanguineous healthy parents from average socio-economic background with one healthy sibling who is 4 years old. There were no previous hospital admissions. Antenatal and post-natal events were uneventful. No antenatal documented infections or radiation exposure. No significant environmental exposure (industrial, Pets).
Examination
The child was found to have moderate acute malnutrition and he was pale. There were generalized lymphadenopathy involving cervical, supratrochlear and bilateral inguinal lymph node groups. No hepatosplenomegaly and the rest of the examination which included a joint examination was resulted normal.
Investigations
In the orthopedic ward, X-rays of the right hip joint, right femur, right knee joint involving tibia and fibular were taken. Blood investigations were conducted, which included a Full Blood Count (FBC) and C - reactive protein (CRP).
X-ray of the tibia showed some periosteal reaction and FBC revealed bicytopenia including leucopenia with moderate neutropenia and anemia (WBC 3.69×106, neutrophil 30% and HB 9.6 g/dl). Platelet count was 216×103/μL and CRP was normal. Following the tests, the child was referred to the general pediatric ward.
A hematological work-up repeated with additional Blood picture, ESR and blood culture.
The red blood cells showed few tear drop cells and were predominantly normocytic, normochromic with few macrocytes. Differential leukocyte count showed 8% blasts, 69% lymphocytes, 17% neutrophils, and 3% monocytes. Platelets were adequate with a count of 213×103/μL with few giant platelets. The platelet indices, namely mean platelet volume and platelet-large cell ratio, were normal.
Bone marrow aspirate smears did not show any particle but were cellular with the presence of 75% lymphoblasts (Figure 1).
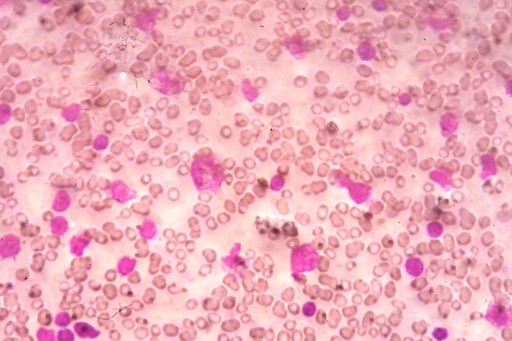
Figure 1. Bone marrow aspirate (Leishman Giemsa, ×1,000). Two hypolobated megakaryocytes seen in a background of many blasts that have a high nucleo cytoplasmic ratio, scant cytoplasm, irregular nuclear membranes, and conspicuous nucleoli.
The blasts were small to medium sized with high nucleo-cytoplasmic ratio and with scanty cytoplasm. There was dispersed chromatin and inconspicuous nucleoli.
The erythroid and myeloid series appeared to be reduced. Few megakaryocytes were seen. Therefore, a diagnosis of acute leukemia was made. These blasts were negative for Sudan black stain and block positivity noted for periodic?acid Schiff (PAS).
On flow cytometry, these blasts showed expression of CD10, CD34, CD19, CD79a, HLA DR, and N Tdt. In addition, blasts were negative for myeloid markers and T-cell markers. A diagnosis of common-ALL-antigen-positive precursor B-cell ALL was reported.
The patient is currently completed the induction phase of chemotherapy and has responded well.
Discussion
Early differentiation of traumatic and non-traumatic limping is difficult to identify, particularly in a small child who has just started walking with a frequent number of falls per day where parents often attribute the limping to a fall or a hypothetical fall.
Patients with ALL often manifest at the time of diagnosis with pancytopenia or bicytopenia but may sometimes have normal peripheral blood cell counts. The platelet series is the earliest and the most consistently decreased series in ALL cases at the time of diagnosis [6].
Decreased platelet counts are often seen at the time of diagnosis (median: 48–52×109/L) [5].
In this case, the patient had 30-40% blasts in bone marrow causing suppression of the erythroid and myeloid series.
In spite of extensive literature review, few cases seem to have been reported. A single study by Hara et al., published in 1990, has reported 36 of 202 children (18%) with ALL to have a platelet count >150×109/μL at diagnosis. Hara et al. found this to be related to the male gender, less marked leukocytosis, less severe anemia, less frequent bleeding manifestations, and a lower percentage of bone marrow blasts [7]. Also it showed that ALL patients without thrombocytopenia had a significantly higher probability of continuous complete remission than those with thrombocytopenia [7].
Therefore, it is important to bear in mind that Acute Leukemia in a small child can initially be expressed as acute limping, with anemia, and/or leukopenia with a normal platelet count. The hematological workup is positively the most sensitive test and any drop in hematopoietic cell counts should be explored immediately by a specialized unit. If the results are normal and a precise diagnosis or cure is not confirmed over time, the blood tests should be repeated and frequent follow-ups should be arranged.
References
2. Sawyer JR, Kapoor M. The Limping Child: A Systematic Approach to Diagnosis. Am Fam Physician. 2009;79(3):215-224.
3. Kim M, Karpas A. Orthopedic emergencies: The limping child. Clin Pediatr Emerg Med. 2002;3:129-137.
4. Beresford MW, Cleary AG. Evaluation of a limping child. Curr Pediatr. 2005;15(1):15-22.
5. Raetz EA, Loh ML, O'Brien MM, Whitlock JA. Acute lymphoblastic leukemia in children. In: Greer JP, Arber DA, Glader B, List AF, Means RT, Paraskevas F, et al., editors. Wintrobe's Clinical Hematology. 13th ed. Philadelphia: Lippincott, Williams and Wilkins; 2014. p. 1616-36.
6. Dewan K, Agarwal K. Acute lymphoblastic leukemia with normal platelet count. Cancer Transl Med. 2015;1:181-2.
7. Hara T, Mizuno Y, Ikuno Y, Okamura J, Nagata M, Ishii E, et al. Acute leukemia with normal platelet count at diagnosis. Acta Paediatr Jpn. 1990;32(5):515-8.
