Abstract
This case report presents the clinical details, diagnostic findings, and management of a 64-year-old female patient who suffered a tibia and fibula fracture, presented in an atypical manner, after twisting her ankle during daily activities. The medical background, physical examination, radiological results, and course of treatment of the patient are detailed. In order to guarantee the best possible recovery and avoid any sequelae, this paper emphasizes the significance of early diagnosis and fast action in the management of such injuries in older adults.
The patient gave written informed consent for the publication of this case study and the photos that go with it.
Keywords
Tibia and fibula fracture, Elderly patient, Diagnostic challenges, Intramedullary nail, External fixation
Background
Fracture of tibia and fibula is not uncommon, especially in elderly people. However, this case presents a unique presentation of leg fracture in the medical landscape. Its uniqueness originates from atypical presentation, diagnostic difficulties, and the management decision made for the patient.
Case Presentation
A 64-year-old woman presented to the Emergency Room (ER) complaining about severe pain and swelling to the left ankle and lower leg. The patient stated that she inadvertently twisted her left ankle (pronation-twist) when she was walking at work. She experienced immediate discomfort and was unable to bear weight on the injured limb, and arrived to the ER in a wheelchair.
The patient stated that she continues to work every day in a nursing home and that she is an active person who rides her bike for about eight km every day. She is awaiting surgery for a total knee replacement in her right knee and has well-controlled hypertension and bilateral osteoarthritis in her knees. Although the patient is not currently getting medication or treatment, osteoporosis is being investigated. She has a BMI of 32.6 but does not smoke or abuse alcohol.
Upon clinical examination, the patient's left ankle exhibited significant swelling along with diffuse discomfort throughout the lateral lower third of the leg and tenderness around the medial malleolus. Both the deformities and the wounds were absent. Applying pressure to the patient's ankle during a squeeze test results in excruciating pain and adjusting the ankle joint caused crepitus. The foot's neurovascular condition was found to be normal.
Diagnostic Evaluation and Treatment
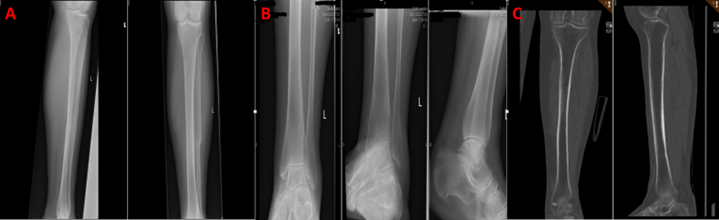
A single comminute midshaft fibula fracture was discovered on standard radiographs and computer tomography (CT) scanning of the leg (Figure 1), with no indications of a tibia fracture or involvement of the knee or ankle. The trauma mechanism suggested a Maisonneuve fracture, as did the midshaft fibula fracture and the tenderness in the medial malleoli.
Figure 1. A & B: Radiographs of the leg showing midshaft fracture fibula with no signs of tibia or knee/ankle involvement. C: CT-scan confirming an isolated midshaft fibula fracture.
After being admitted to the orthopedic ward, the patient's syndesmotic stability was evaluated through surgery. Nevertheless, a trauma surgeon assessed the ankle intraoperatively using fluoroscopy and discovered that it was stable. The syndesmosis was undamaged, and no additional fractures were seen. A conservative strategy (isolated fibula fracture without syndesmosis damage) was selected with walker brace for 4-6 weeks and was instructed to start mobilization with full weight-bearing on the injured leg, which the patient was able to do upon discharge from hospital.
Complication and Management
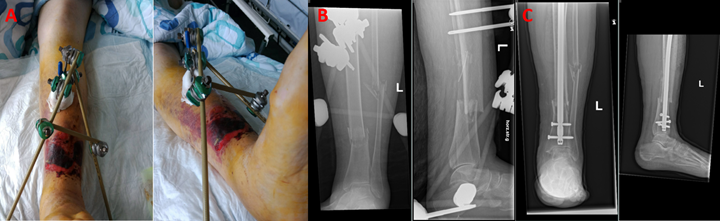
Five days later, the patient came back to the emergency room (Figure 2A) with large blisters, discoloration, swelling, and leg deformity. The patient followed instructions to bear weight but did not report any new trauma. After obtaining new radiographs, it was discovered that the patient had sustained a distal third transverse tibia and fibula fracture. The fracture had resulted in a shortening of over 2 cm, as well as a posterior displacement of the distal fragment of about half a bone's width and increased posterior angulation (Figure 2B).
Figure 2. A: Swelling and large bullae with hematomas of a large portion of the lower limb. B: X-ray of the lower leg seen with a lower third transverse tibia fracture with shortening of more than 2 cm and a posterior displacement and angulation of the distal tibia.
The patient was brought straight to the operating room. In order to stabilize the fracture, achieve realignment, and relieve soft tissue pressure from the fractured bone, external fixation was chosen due to the swelling of the soft tissues and the potential for skin necrosis (Figure 3).
Leg elevation, pain management, prophylactic antibiotics, daily soft tissue examination, dressing changes, and compression were the patient's post-operative treatments. The patient underwent definitive surgery with a tibia locking intramedullary nail eight days later, after tissue swelling had decreased (Figure 3C).
Figure 3. A & B: Images and radiographs of the post-operative external fixation. C: Post-operative radiograph after final surgery with intramedullary locking nail placement.
Due to her poor balance, the patient was prescribed a walker and instructed to limit their weight-bearing on the injured limb for six weeks after surgery. Exercises for rehabilitation and physical therapy were started in order to avoid stiffness and encourage functional recovery. The program's objectives were to reduce pain, increase range of motion, and strengthen the surrounding muscles. Three days following surgery, the patient was discharged.
Follow-up: Following surgery, the patient was scheduled for routine follow-up appointments at two and six weeks to assess healing, fracture alignment, and modify the rehabilitation regimen. The patient was also instructed to get in touch with her general practitioner to start an osteoporosis investigation.
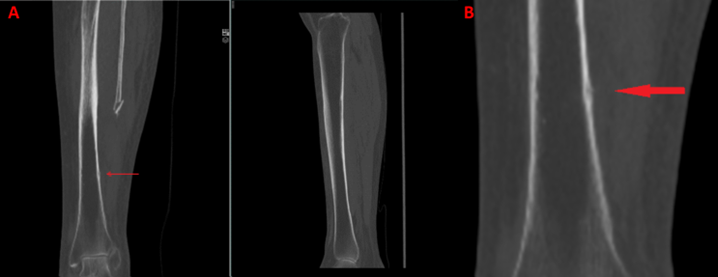
After reviewing the initial CT scan again that was taken before fracture displacement, a small cortical incongruence in the tibia few centimeters distal to the fibula fracture can be seen on one single segment of the coronal CT scan image (Figure 4). In hindsight, this is most likely what caused the tibia to completely fail, resulting in a displaced lower leg fracture.
Figure 4. A & B: CT-scanning AP segment shows possible cortical crack in the lat. border of tibia few centimeters below fibula fracture, which in retrospect, was the cause of the midshaft tibia fracture later on.
Discussion
Fractures of the tibia shaft are the most common long bone fractures, with incidence of 16.9/100,000/year [1]. Most of these fractures are seen in young males (thought to be related to sports or from a direct, high-energy mechanism of injury like motor vehicle accidents) with a second peak of incidence among elderly patients, whose injuries mostly result from lesser/minor trauma or fall [2]. Living tissue, such as bone, is continually being replaced and broken down. When new bone is not growing to replace lost bone, the condition known as osteoporosis develops. Bones affected by osteoporosis become weak and brittle, easily breaking from simple stresses like bending over or falling. Even though spiral, nondisplaced fracture patterns with little soft tissue damage are typically caused by indirect, torsional, low-energy injury mechanisms, older patients with osteoporotic bone may experience more complex patterns. The main reason for this is the changes to bone mass caused by osteoporosis, which is common among the over 50s [2]. Women who are over 50 years have approx. 50% risk of low bone density mass which is considered as precursor for osteoporosis. In osteoporosis the bones demonstrate deterioration in microarchitecture, leading to loss of bone mineral density and increased risk of a fracture with minor trauma [4].
This case demonstrated the difficulties in identifying and treating atypical fractures in elderly patients, as well as the delayed manifestation of a transverse tibia shaft fracture, five days after initial treatment [3]. The question arises, whether we could have done more for this patient, but we would argue that the patient was treated with the full scope of clinical examinations, available imaging, syndesmotic testing with fluoroscopy under general anesthesia, and the patient performed full weight bearing on the day of discharge. In retrospect, an array of doctors oversaw a small cortical infraction, and this highlights the importance of possibly continuing with further investigations if the trauma mechanism and clinical examination do not coincide with the imaging findings.
Conclusion
This type of fracture after minor trauma is due to osteoporosis or low bone density and the possibility of underlying cortical changes or small cracks in tibia cortex after a relevant trauma should raise alarms, and trauma surgeons should possibly hold back with weight bearing until a clinical follow-up can be performed shortly after. Trauma surgeons should be cautious of atypical fractures because the population is getting older and therefore more susceptible, particularly in patients with osteoporotic bones.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Consent obtained from the patient.
Availability of data and material
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study. For more information contact the corresponding author Esam Lawand, Email: elaw@regionsjaelland.dk
Competing interests
The authors declare that they have no competing interests.
Funding
This case study has been conducted without external funding.
Authors' contributions
Esam Lawand first Author, Jacob F. Mortensen second Author (revised the work), Michael Krasheninnikoff second author (revised and approved the study report).
Acknowledgements
Not applicable.
References
2. Courtney PM, Bernstein J, Ahn J. In brief: closed tibial shaft fractures. Clin Orthop Relat Res. 2011 Dec;469(12):3518-21.
3. Pinto A, Berritto D, Russo A, Riccitiello F, Caruso M, Belfiore MP, et al. Traumatic fractures in adults: missed diagnosis on plain radiographs in the Emergency Department. Acta Biomed. 2018 Jan 19;89(1-S):111-123.
4. Wright NC, Looker AC, Saag KG, Curtis JR, Delzell ES, Randall S, et al. The recent prevalence of osteoporosis and low bone mass in the United States based on bone mineral density at the femoral neck or lumbar spine. J Bone Miner Res. 2014 Nov;29(11):2520-6.