Abstract
Aims: To identify follow-up rate and evaluate the endodontic outcome and their association with technical quality of root canal therapy (RCT) done by dental undergraduates.
Method: Technical quality of RCT and follow-up rate visits of 350 teeth from 272 patients after RCT done by dental undergraduates were evaluated retrospectively from year 2012 to 2015 using the electronic records. These patients were recalled to assess the clinical, radiographic and overall endodontic outcome. Clinical and radiographic examinations were done following the criteria in compliance with standards guidelines. Each RCT was considered successful when clinical and radiographical findings were satisfactory. Association between technical quality of RCT and endodontic outcome was analysed using chi-square test.
Results: The retrospective electronic records revealed only 16% of follow-up rate and 59 (21.7%) patients attended the recall visits and 90 teeth (25.7%) of these patients were assessed. The clinical, radiographic, endodontic success, and acceptable technical quality of RCT were observed in 72.2%, 85.6%, 60.7%, and 51.1% respectively. There was no significant association observed in between technical quality of RCT and endodontic outcome (p=0.10).
Conclusions: The follow-up rate visits done by dental undergraduates after completion of RCT was low. The success rate of RCT performed by dental undergraduates was 66.7% with no significant association in between the technical quality of RCT and endodontic outcome.
Keywords
Clinical audit, Endodontic follow-up, Endodontic outcome, Technical quality
Clinical Relevance
• Clinicians need to understand the importance of clinical audit and take the necessary remedial actions to enhance their knowledge and skills to carry out clinical audit and improve the outcome.
• Clinicians also need to recognize the importance of follow-up and emphasize on it to improve the long-term success of RCT.
Introduction
A successful root canal therapy (RCT) depends on the accuracy of diagnosis, treatment planning, thorough debridement of the root canal system, three dimensional root canal filling, good coronal seal, and follow up [1]. The success of RCT can be evaluated by the clinical and radiographic outcomes . According to the quality guidelines from the consensus report of endodontic treatment from European Society of Endodontology 2006, the findings such as absence of pain, swelling and other symptoms, sinus tract, loss of function and presence of radiological evidence of a normal periodontal ligament space around the root indicate a favourable outcome [1]. Pre-operative absence of periapical radiolucency, root filling with no voids, root filling extending to 2 mm within the radiographic apex and satisfactory coronal restoration have shown to play a major impact on the endodontic outcome [2-6]. In studies correlating the technical quality of root filling and the endodontic outcomes, it has been reported that teeth with inadequately filled root canals revealed presence of periapical pathosis more often than teeth with adequately filled root canals [7]. According to a study conducted by Song et al., teeth with both adequate root fillings and coronal restorations showed a significantly better endodontic outcome (82%) [8]. Similarly, Cakici et al. reported that the quality of both the root filling and coronal restoration affect the periapical health of root-filled teeth [ 9]. In contrast, Da Silva et al. did not find any significant association between the quality of the root filling and the presence of periapical lesion in the Australian population and factors, such as the coronal restoration quality, should be further investigated as suggested [10]. Follow-up after RCT completion is important to determine the outcome of endodontic treatment. Many guidelines have reported the recommended follow-up interval but study evaluating the follow-up visits done by dental undergraduates is very limited [1]. By providing follow-ups, clinicians are able to deduce and solve the post-operative problem which can adversely affect a patient’s quality of life in the long run. As suggested by Lopes and Siqueira Jr [11], the outcome of RCT should be evaluated every six months. This helps to depict the normal or altered condition of the periapical tissues.
In the attempts to evaluate the quality of the RCT, several studies have been done however, most of studies have focused on assessing the technical quality of the root canal fillings or endodontic outcome without correlating the relationship between the technical quality and the endodontic treatment outcomes. Therefore, the purpose of this study was to identify the follow-up rate done by dental undergraduates, determine the endodontic outcome (clinical and radiographic outcomes) of root canal treated teeth performed by dental undergraduates and evaluate the association in between the endodontic outcome with the technical quality of RCT.
Materials and Methods
Fourth year dental undergraduates at the International Medical University had clinical audit training as part of their curriculum, which involved a classroom plenary on the principles and methodologies of clinical audit and a seminar in which groups of six students present their audit protocols for different dental disciplines. Retrospective electronic and digital radiographic records from January 2012 until December 2015 were retrieved from the electronic software records (Open Dental) of all teeth that were endodontically treated by dental undergraduates in the Oral Health Centre of the International Medical University, Kuala Lumpur, Malaysia. Teeth having pre-operative and post-operative radiographs were included, and the records of treatment that have yet to be completed or were lacking post-operative radiographs were excluded from the study. All RCT performed by dental undergraduates followed a standard hybrid method using K-files for all cases as reported previously by Wong et al. [12]. The rate of followup done by dental undergraduates after completion of RCT was evaluated using these electronic records. The electronic records were analysed to gather the information whether the patient after completing the RCT was recalled for follow-up and the clinical and radiographic outcomes were assessed and recorded.
The examiners underwent a training from trained endodontists on evaluation of the clinical and radiographic endodontic outcomes prior to the study. The pilot study was carried out using 10 patients and all observations were performed by the examiners and endodontists independently. Inter-observer reliability test was carried out using Cohen’s Kappa test. A final consensus was reached when the inter-rater agreement kappa value was found to be within almost perfect agreement (0.81-099).
These 272 patients who had undergone RCT earlier by dental undergraduates were called to assess the clinical and radiographic outcomes. Maximum three phone calls were made at the interval of one week for each patient. A total 59 (21.7%) out of 272 patients agreed to come for the recall visits. Those, who did not attend the recall appointments, were asked to answer the telephone questionnaire to evaluate the endodontic outcome. The reasons for not attending the recall visits were also recorded and analysed.
A detailed checklist regarding the clinical and radiographic outcomes (Table 1) was formulated based on the guidelines done by the European Society of Endodontology [1] and American Association of Endodontists [13]. In clinical outcomes, the presence of tenderness to percussion or palpation, swelling, sinus tract, locally deep periodontal probing defect, tooth mobility and the condition of coronal seal were evaluated, while in radiographic outcomes, the presence of static or expanding periapical lesion and absence of root fracture or resorption were evaluated. Each RCT was considered successful when it meets the satisfactory outcomes both clinically and radiographically. As for multi-rooted teeth, all canals were evaluated simultaneously (e.g. A multi-rooted tooth was considered radiographically satisfactory only when the radiographic outcomes of all the root canals were satisfactory).
| Satisfactory | Unsatisfactory | ||
| Clinical Outcome | |||
| 1. | Tenderness to percussion or palpation | Absent | Present |
| 2. | Presence of soft tissue swelling | Absent | Present |
| 3. | Presence of sinus tract | Absent | Present |
| 4. | Presence of locally deep periodontal probing defect | Absent | Present |
| 5. | Increased tooth mobility | Absent | Present |
| 6. | Clinical condition of the tooth | Permanent coronal restoration with no sign of apparent leakage | Teeth without permanent coronal restoration; with permanent restoration presenting apparent leakage; with coronal fracture |
| Radiographic Outcome | |||
| 1. | Static or expanding periapical lesions | Absent | Present |
| 2. | Root fracture or resorption | Absent | Present |
Clinical examination was done based on respective criteria [1,13] and periapical radiograph was taken for each patient. Two examiners evaluated all the clinical and radiographic outcomes independently. Digital radiographs (preoperative and postoperative) were examined in the form of full screen images that could be enhanced and zoomed in on the computers using VixWin Platinum software (Gendex Dental Systems, Hatfield, PA, USA). Both preoperative and postoperative radiographs of each patient were examined by the same observers in a darkened environment to ensure the reliability and reproducibility of results.
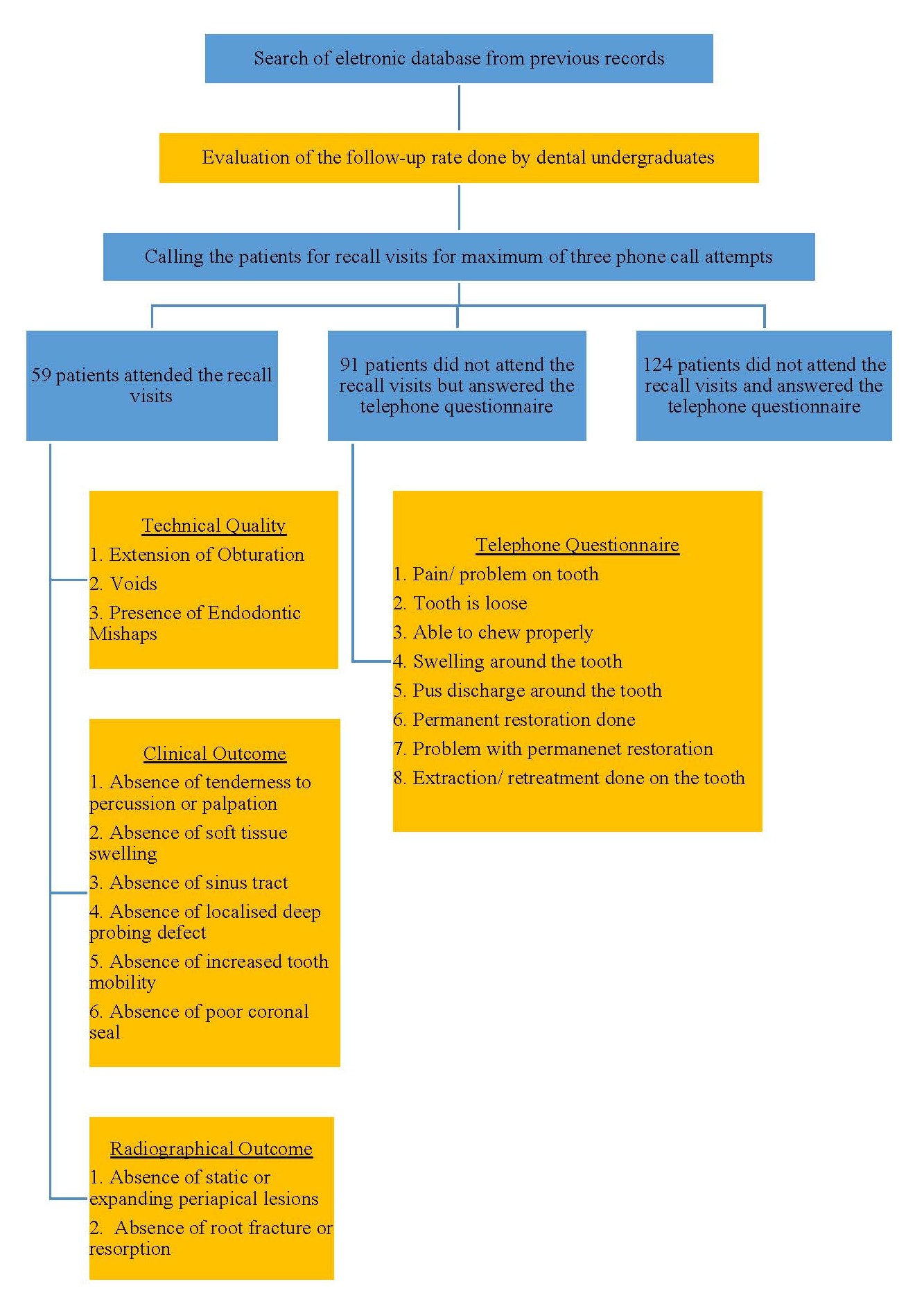
Data was tabulated and analyzed. The frequency distributions of the endodontic success and failure were calculated. The technical quality of each tooth underwent RCT was also observed, which included the extension of obturation, presence of voids and endodontic mishaps. The technical quality of the RCT performed by dental undergraduates in single-rooted teeth was compared in multi-rooted teeth. The association in between technical quality of RCT and endodontic outcome was analysed by using chi square test from SPSS Statistical Software (Version 21, Inc., Chicago, IL, USA). Figure 1 shows the summary of the methodology.
Figure 1. Methodology Summary.
Results
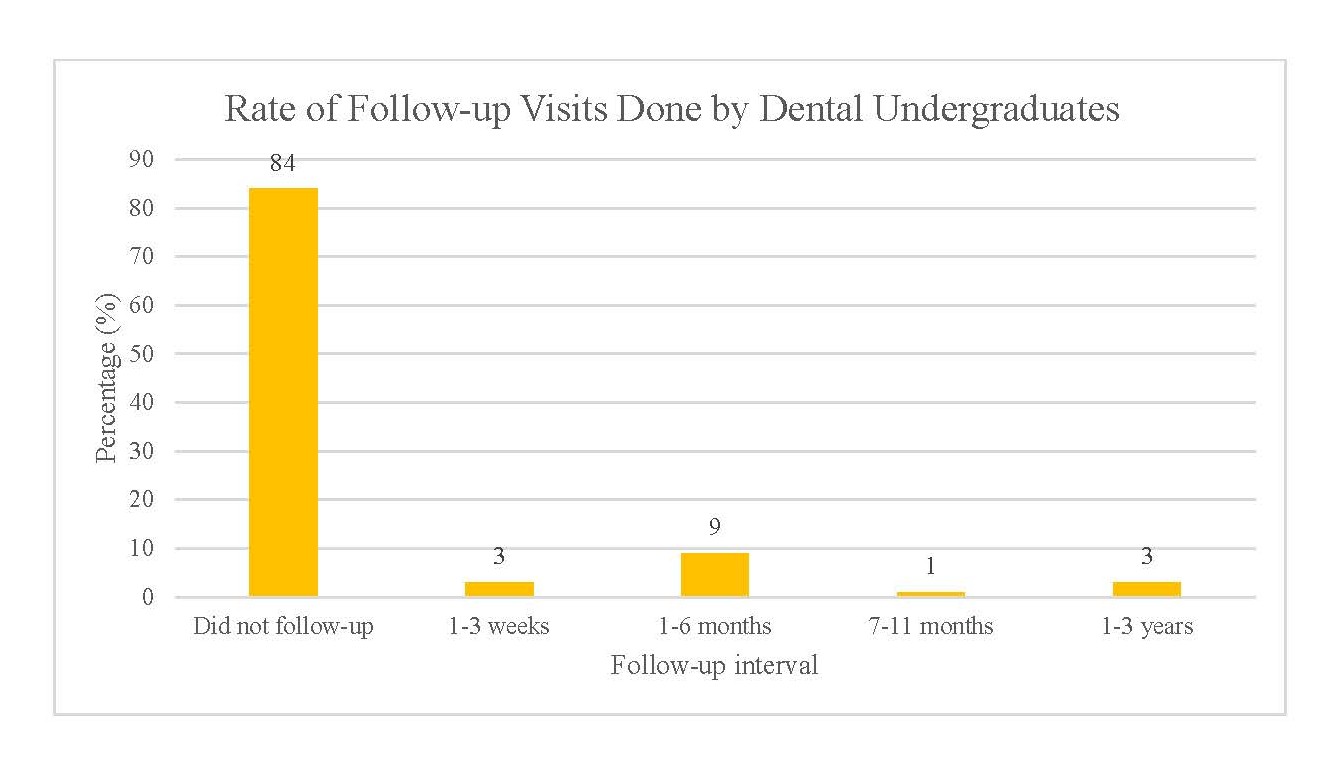
The rate of follow-up visits done by dental undergraduates was low (16%). 84% of the dental undergraduates did not call the patients for follow-up after RCT completion. For those who arranged follow-up visits, majority of followup were done in 1- and 2-months’ time after RCT (Figure 2). Out of 272 patients contacted, 59 (21.7%) patients presented to the clinic for the recall visits. A total of 90 (25.7%) RCT teeth were included in the study. The mean of recall period for this study was 2.8 years, ranging from 1 to 6 years. The characteristics of patients (gender and aged group) and tooth type are presented in Table 2. The data revealed that mainly females (66.7%) attended the recall visits and the type of teeth included were mostly premolars (50%). 65 teeth (72.2%) had clinical success and 77 teeth (85.6%) were considered as radiographic success. A total of 60 teeth (66.7%) were considered as overall success as they have adequate successful outcomes in both clinically and radiographically. The results of each criterion for clinical and radiographic outcome assessment are presented in Table 3. Out of 31 single-rooted teeth, 12 teeth (38.7%) showed acceptable technical quality of RCT, while out of 59 multi-rooted teeth, 33 of them (55.9%) showed acceptable technical quality of RCT. The cross tabulations of technical quality of root canal filling and endodontic outcome are presented in Table 4 and there was no statistically significant association observed (p>0.05). However, root canal fillings with apical extension within 2 mm from the radiographic apex showed the highest success rate (60%).
Figure 2. Rate of follow-up visits done by dental undergraduates after completion of RCT.
| Patients who attended the recall visits | Patients who did not attend the recall visits but answered the telephone questionnaire, n (%) | Patients who did not attend the recall visits and did not answered the telephone questionnaire, n (%) |
|||
|---|---|---|---|---|---|
| Endodontic success, n (%) | Endodontic failure, n (%) | Total, n (%) | |||
| Gender | |||||
| Male | 19 (21.1%) | 11 (12.2%) | 30 (33.3%) | 48 (52.7%) | 73 (42.6%) |
| Female | 41 (45.6%) | 19 (21.1%) | 60 (66.7%) | 43 (57.3%) | 96 (57.4%) |
| Age group | |||||
| 18-39 years old | 6 (6.7%) | 0 (0%) | 6 (6.7%) | 30 (32.9%) | 54 (32.0%) |
| 40-59 years old | 37 (41.1%) | 15 (16.7%) | 52 (57.8%) | 45 (49.5%) | 75 (44.4%) |
| 60-80 years old | 17 (18.9%) | 15 (16.7%) | 32 (35.5%) | 16 (17.6%) | 40 (23.6%) |
| Tooth type | |||||
| Incisor | 14 (15.6%) | 10 (11.1%) | 24 (26.7%) | 25 (27.5%) | 43 (25.4%) |
| Canine | 5 (5.6%) | 2 (2.2%) | 7 (7.8%) | 10 (10.9%) | 22 (13.0%) |
| Premolar | 30 (33.3%) | 15 (16.7%) | 45 (50%) | 37 (40.7%) | 65 (38.5%) |
| Molar | 11 (12.2%) | 3 (3.3%) | 14 (15.5%) | 19 (20.9%) | 39 (23.1%) |
| Total | 90 | 91 | 169 | ||
| n: number of teeth | |||||
| Criteria | n | % |
|---|---|---|
| Clinical satisfactory | 65 | 72.2 |
| 1. Absence of tenderness to percussion or palpation | 81 | 90 |
| 2. Absence of soft tissue swelling | 88 | 97.8 |
| 3. Absence of sinus tract | 88 | 97.8 |
| 4. Absence of probing defect | 76 | 84.4 |
| 5. Absence of increased tooth mobility | 76 | 84.4 |
| 6. Absence of poor coronal seal | 85 | 94.4 |
| Radiographic satisfactory | 77 | 85.6 |
| 1. Absence of static/expanding periapical lesions | 78 | 86.7 |
| 2. Absence of root fracture/resorption | 89 | 98.9 |
| Endodontic success | 60 | 60.7 |
| n: number of teeth; %: percentage | ||
| Clinical outcome n (%) | Radiographic outcome n (%) | Endodontic outcome n (%) | ||||
|---|---|---|---|---|---|---|
| S | U | S | U | S | U | |
| Extension of obturation | ||||||
| Within limits (n=80) | 59 (65.6) | 21 (23.3) | 69 (76.7) | 11 (12.2) | 54 (60) | 26 (28.9) |
| Not within limits (n=10) | 6 (6.7) | 4 (4.4) | 8 (8.9) | 2 (2.2) | 6 (6.7) | 4 (4.4) |
| P value | 0.36 | 0.60 | 0.64 | |||
| Voids | ||||||
| Absent (n=62) | 42 (46.7) | 20 (22.2) | 52 (57.8) | 10 (11.1) | 38 (42.2) | 24 (26.7) |
| Present (n=28) | 23 (25.6) | 5 (5.6) | 25 (27.8) | 3 (3.3) | 22 (24.4) | 6 (6.7) |
| P value | 0.16 | 0.50 | 0.11 | |||
| Endo mishap | ||||||
| Absent (n=61) | 42 (46.7) | 19 (21.1) | 52 (57.8) | 9 (10) | 38 (42.2) | 23 (25.6) |
| Present (n=29) | 23 (25.6) | 6 (6.7) | 25 (27.8) | 4 (4.4) | 22 (24.4) | 7 (7.8) |
| P value | 0.30 | 0.90 | 0.20 | |||
| Overall technical quality | ||||||
| Acceptable (n=45) | 30 (33.3) | 15 (16.7) | 37 (41.1) | 8 (8.9) | 26 (28.9) | 19 (21.1) |
| Unacceptable (n=45) | 35 (38.9) | 10 (11.1) | 40 (44.4) | 5 (5.6) | 34 (37.8) | 11 (12.2) |
| P value | 0.24 | 0.37 | 0.10 | |||
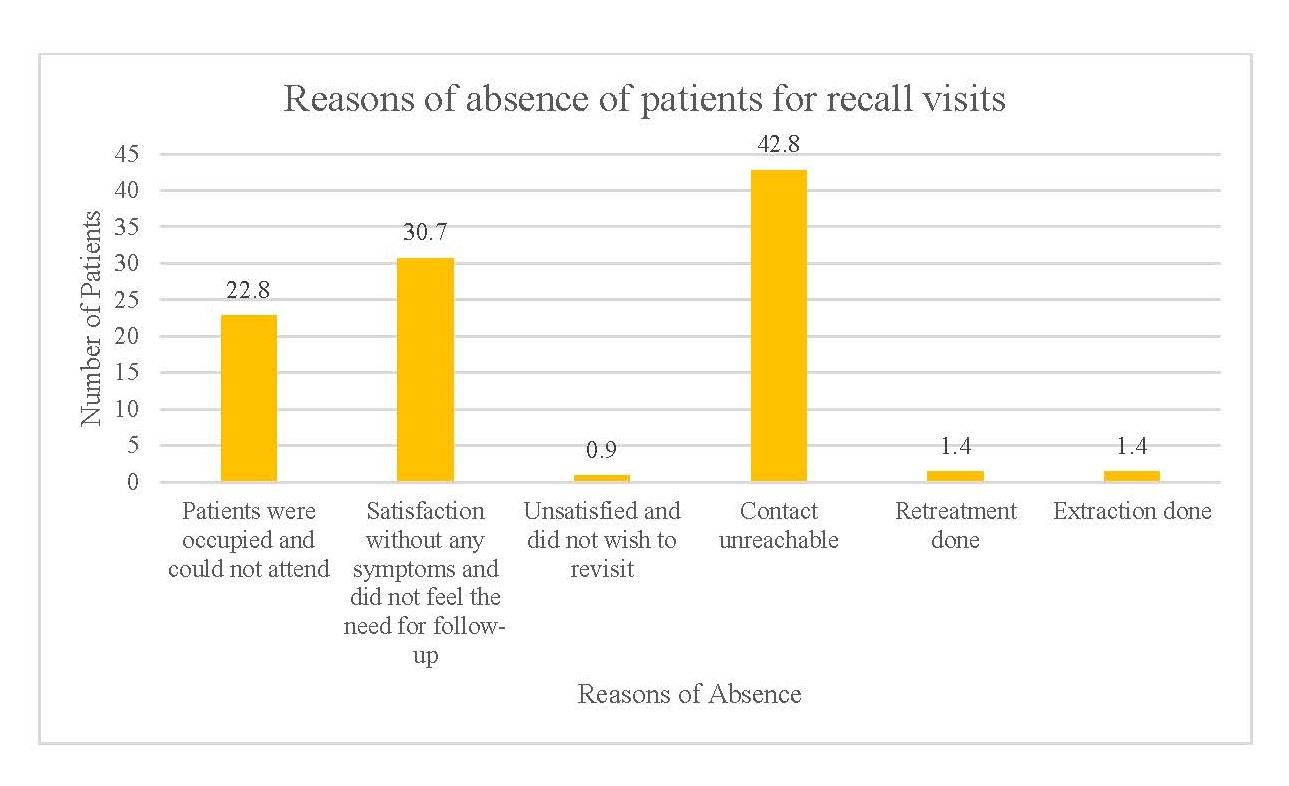
Among the patients (n=272) contacted, 213 (78.3%) patients could not attend the recall visits. The reasons of absence are presented in Figure 3. The main reasons for their absence were unreachable contact (42.8%), followed by patients expressed satisfaction without any symptoms (30.7%) and did not feel the need for follow-up (22.8%). A total of 91 out of 215 patients responded to the questionnaire for absentees and the results were tabulated in Figure 4.
Figure 3. Reasons of absence of patients for recall visits.
Figure 4. Result of telephone questionnaire for absentees.
Discussion
Clinical audit has found to be an important tool and through clinical audit, the overall performance of dental undergraduates including the follow-up rate done for patients after their endodontic treatment can be evaluated. Based on the results of the present audit, dental undergraduates were reinstructed to follow up their endodontic cases for at least one year, according to the recommended guidelines by European Society of Endodontology [1] and American Association of Endodontists [13]. During the one-year follow-up visit, the dental undergraduate needs to examine the patient clinically, radiographically and record the findings/ outcomes to satisfy all the requirements needed to complete an endodontic case necessary for their expected clinical competence.
A study [14] has shown that clinical audit encourages individual general dental practitioners to evaluate and improve their practice from different aspects, and to reevaluate areas which were previously audited in order to maintain high quality of service. The importance and benefits of clinical audit has also been emphasized in a study done by Fong et al. [15] who suggested that clinical audit-feedback cycle is an effective educational tool for improving dental undergraduates’ compliance with record keeping and performance in the technical quality of RCT.
To understand the perspective of patients towards follow-up, all patients who came back for recall visits were interviewed to gather their feedbacks regarding the visit. Among testimonials given by the patients, most of them responded with gratitude and satisfaction because clinicians are concerned about their oral health years after completing the treatment. Majority hope that such followup visits can be carried out regularly in the future. However, there were patients who refused returning for follow-up with reasons such as busy with work, having no problem with their root treated teeth and not understanding the need of follow-up. Hence, patients should be motivated, educated, and informed to attend periodic follow-ups. Treatment should not be considered as complete until follow-ups are done. The importance of follow-up should be emphasized not only to the patients but also to the clinicians because it eventually allows clinicians to review the endodontic outcome and identify the need of improvement. Vena et al. [16] demonstrated that during follow-up visits, several patients reported persistent pain, which lasted up to five years after RCT. By providing follow-ups, clinicians are able to deduce and solve the post-operative problem which can adversely affect a patient’s quality of life in the long run. According to Travassos et al. [17], a period of two to five years is necessary to observe complete repair. Some authors claimed that a follow-up radiograph, which will show either normal healing processes or signs of failure, should be taken every six months for two years [18].
The present study allowed the evaluation of the outcome of RCT performed by undergraduate students in a dental school in Malaysia. A systematic review and meta-analysis of 63 outcome studies from 1922 to 2002 showed that the mean pooled success rate at least one year after primary endodontic treatment was 74.7%, with a range of 68% to 85% success rate, when strict criteria (which is, lack of periapical radiolucencies) was applied; when loose criteria (that is, reduction in periapical radiolucency) was applied, the mean success rate was 85.2% with a range of 60% to 100% success rate [19]. In the current study, the absence of static or expanding periapical radiolucency and the absence of root fracture or resorption were considered as radiographical satisfactory, which is in the category of loose criteria.
Dental undergraduates in the current study achieved an endodontic success rate of 66.7% after an average of 2.8 years follow-up, which was lower as compared to the dental undergraduates in other countries [20-23] and similar to Ng et al. [19]. In UK, Heling and Tamshe [20] reported an overall success rate of 70% in 213 teeth that were treated by dental undergraduates. Greek [21] and Brazil [22] dental schools showed a success rate of 72.8% and 75.5% respectively in their follow-up three years after the completion of RCT. Smith et al. [24] demonstrated an overall success rate of 84% in 821 teeth that had root fillings placed by postgraduate students and staff in a dental hospital while Barbakow et al. [25] revealed 87% success rate in RCT performed in a general practice. Among these studies, the success rate was higher in RCT performed by postgraduate students and general dental practitioners as compared to undergraduate students. This shows that the number of year of experience in addition to the difficulty level of the case in practising may influence the endodontic outcome.
In the current study, the presence of tooth mobility and the localized deep probing depth were the highest while the presence of soft tissue swelling, and sinus tract were the lowest among the clinical outcomes. This can be explained as patients with symptoms, such as pain, swelling or having foul smell, would have gone back to the previous follow-up arranged or called up for appointments to review. On the other hand, mild tooth mobility and localized deep probing depth can only be assessed clinically by the clinicians and cannot be detected by the patients themselves.
Another objective of present study was to evaluate the correlation between the technical quality of endodontic treatment and the endodontic outcome. In preliminary work [15], the technical quality of RCT was assessed in terms of apical extension of obturation, presence of void in the root canal fillings and presence of endodontic mishaps. Combining results from preliminary work and current study, there was no statistically significant correlation between the technical quality and the endodontic outcomes. In contrast, several studies had found significant association between the two [25,27-29]. A study evaluating 1,372 periapical radiographs of root treated teeth also displayed that teeth with poor root canal filling had higher apical periodontitis prevalence (66.3%) than those with adequate root canal filling (16.5%) [ 26] . According to Polyzos et al. [21], the success rate for root canal with and without voids were 45.9% and 83.3% respectively (p<0.001). These results are in agreement with the study done by Tronstad et al. [30], whereby they demonstrated that the factor of utmost importance for periapical health status is the technical quality of RCT. This discrepancy could be due to the limited number of patients’ assessment in the present study. However, the present result was in accordance with Benvenutti et al. [ 23] who revealed that poor condensation of root canal filling had no association with the failure of root canal therapy. To justify the result of this study, it is believed that reasons other than technical quality of RCT may affect the endodontic outcome. Determinants of endodontic outcome includes precision of diagnosis, maintenance of the aseptic chain, knowledge of the anatomy of root canal system, correct biomechanical preparation, an adequate coronal restoration, and the periodic treatment follow-up [ 26,31 ]. In fact, data retrieved from a retrospective clinical study showed that the quality of coronal restoration carried a greater impact on endodontic outcome than the quality of RCT. It was suggested that a favourable outcome can be achieved even in poorly-filled root canals when there is adequate coronal restoration [32]. On the other hand, necrotic pulp tissue contains microorganisms which are not necessarily found in vital pulp, leading to comparatively lower success rate [23]. Teeth with vital pulp were observed to have higher cumulative success rate than those with non-vital pulp, indicating that the pulp space of non-vital teeth is often infected [33].
Even though the current study showed statistically insignificant correlation between technical quality and endodontic outcome, the apical extension of root canal fillings within 2 mm from the radiographic apex was found associated with the highest success rate of endodontic outcome (67.5%), which is consistent with other studies [21,25,27,34-36]. The present study also reported highest failure rates in unacceptable apical extension of obturation (40%) as compared to presence of void (21.4%) and endodontic mishaps (24.1%). This may be explained by insufficient apical debridement or accumulation of contaminated dentin, which can induce persistent infectious agents in the root apexes when there is underextension of root canal filling, leading to higher prevalence of endodontic failure [37]. In line with the present study, Heling et al. [34] also observed that the apical limit of root canal obturation affects the success rate of RCT and higher failure rates was shown in those root canals obturated beyond the apex. In terms of extension of root canal filling, another study demonstrated that success rate of root filling extended by 0-2 mm from the radiographic apex (86.9%) was significantly higher (p<0.001) than those under-filled or overfilled roots (58.4%) [21].
In the present study, poor condensation leading to void in the root canal fillings was associated with the highest success rate (78.6%) than presence of endodontic mishaps (75.9%) and unacceptable apical extension of the obturation (60%), which is in agreement with a study done by Benvenutti et al. [23]. A systematic review done by Ng et al. [38] also found one study having reported a 68% survival rate of teeth with voids in their root fillings at 5 and 10 years.
In the current study, the rate of acceptable technical quality of RCT was lower in single-rooted teeth (38.7%) as compared to in multi-rooted teeth (55.93%), which was inconsistent with studies done by Khabbaz et al. [3], Balto et al. [39], and Moussa-Badran et al. [40]. In the present study, most single-rooted teeth RCT were performed by third year dental undergraduates which have lesser experience, while most multi-rooted RCT were done by fourth and fifth year dental undergraduates. The other reason for higher acceptable rate of technical quality of RCT in multi-rooted teeth could be due to close supervision and proper case selection as multi-rooted teeth with minimum difficulty were allowed to be done by dental undergraduates.
However, there were a few limitations while performing this study. The sample size was small as most patients could not make it for the recall visits. To overcome the lack of sample size, questionnaire through phone call was done for each patient who was absent. Questions regarding pain, swelling, mobility, problem with eating, and pus discharge on the root canal treated tooth; type and condition of restoration were asked. Besides, other factors that will influence the endodontic outcome such as a lack of diagnosis in patients’ records were not taken into consideration. Meanwhile, patients with medical conditions were not excluded from the study. Lastly, by using two-dimensional periapical radiograph on a threedimensional structure, it limits the actual radiographic evaluation of a root canal treated tooth.
Conclusion
The rate of follow-up visits done by dental undergraduates after completion of RCT was low and the success rate of RCT performed by dental undergraduates was 66.7%. Thus, importance of follow-up of RCT needs to be emphasized to assess the endodontic outcome, evaluate the need of improvement and ensure patients’ satisfaction.
Acknowledgements
Special thanks to all the patients who took effort to attend the follow-up appointment.
Competing Interest
The authors declared no competing interests.
References
2. Whitworth J. A retrospective study of root canal treatment in the armed forces. British Dental Journal. 2001 Feb;190(3):136.
3. Khabbaz MG, Protogerou E, Douka E. Radiographic quality of root fillings performed by undergraduate students. International Endodontic Journal. 2010 Jun;43(6):499-508.
4. Tarim Ertas E, Ertas H, Sisman Y, Sagsen B, Er O. Radiographic Assessment of the Technical Quality and Periapical Health of Root-Filled Teeth Performed by General Practitioners in a Turkish Subpopulation. The Scientific World Journal. 2013;2013:1-7.
5. Dadresanfar B, Akhlaghi NM, Vatanpour M, Yekta HA, Mohajeri LB. Technical quality of root canal treatment performed by undergraduate dental students. Iranian Endodontic Journal. 2008;3(3):73-8.
6. Ng YL, Mann V, Rahbaran S, Lewsey J, Gulabivala K. Outcome of primary root canal treatment: systematic review of the literature–Part 2. Influence of clinical factors. International Endodontic Journal. 2008 Jan;41(1):6-31.
7. Ilgüy D, Ilgüy M, Fisekçioglu E, Ersan N, Tanalp J, Dölekoglu S. Assessment of root canal treatment outcomes performed by Turkish dental students: results after two years. Journal of Dental Education. 2013 Apr;77(4):502-9.
8. Song M, Park M, Lee CY, Kim E. Periapical status related to the quality of coronal restorations and root fillings in a Korean population. Journal of Endodontics. 2014 Feb 1;40(2):182-6.
9. Cakici EB, Yildirim E, Cakici F, Erdogan AS. Assessment of periapical health, quality of root canal filling, and coronal restoration by using cone-beam computed tomography. Nigerian Journal of Clinical Practice. 2016;19(5):673-7.
10. Da Silva K, Lam JM, Wu N, Duckmanton P. Crosssectional study of endodontic treatment in an Australian population. Australian Endodontic Journal. 2009 Dec;35(3):140-6.
11. Lopes HP, Siqueira Junior JF. Endodontia: biologia e técnica. 3. ed. Rio de Janeiro: Guanabara Koogan; 2010: 645-91.
12. Wong CY, Liaw YX, Wong JZ, Chen LC, Parolia A. Factors associated with the technical quality of root canal fillings performed by undergraduate dental students in a Malaysian Dental School. Brazilian Journal of Oral Sciences. 2016 Oct 13;15(1):45-50.
13. Competence in the Diagnosis of Endodontic Treatment. American Association of Endodontists. 2017: 1-11.
14. Simons D, Williams D. Can audit improve patient care and treatment outcomes in endodontics?. British Dental Journal. 2013 May;214(9):456-9.
15. Fong JY, Tan VJ, Lee JR, Tong ZG, Foong YK, Tan JM, et al. Clinical audit training improves undergraduates’ performance in root canal therapy. European Journal of Dental Education. 2018 Aug;22(3):160-6.
16. Vena DA, Collie D, Wu H, Gibbs JL, Broder HL, Curro FA, et al. Prevalence of Persistent Pain 3 to 5 Years Post Primary Root Canal Therapy and Its Impact on Oral Health–Related Quality of Life: PEARL Network Findings. Journal of Endodontics. 2014 Dec 1;40(12):1917-21.
17. Travassos RM, Caldas Junior AD, Albuquerque DS. Cohort study of endodontic therapy success. Brazilian Dental Journal. 2003;14(2):109-13.
18. Antunes LS, Souza CR, Salles AG, Gomes CC, Antunes LA. Does Conventional Endodontic Treatment Impact Oral Health-related Quality of Life? A Systematic Review. European Endodontic Journal. 2018;3(1):2-8.
19. Ng YL, Mann V, Rahbaran S, Lewsey J, Gulabivala K. Outcome of primary root canal treatment: systematic review of the literature–part 1. Effects of study characteristics on probability of success. International Endodontic Journal. 2007 Dec;40(12):921-39.
20. Heling B, Tamshe A. Evaluation of the success of endodontically treated teeth. Oral Surgery, Oral Medicine, Oral Pathology. 1970 Oct 1;30(4):533-6.
21. Polyzos NK, Sarris KG, Pita AI, Mikrogeorgis GV, Lyroudia KM. Factors Affecting the Outcome of Non-Surgical Endodontic Treatments Performed by Undergraduate Students in a Greek Dental School. European Endodontic Journal. 2018;3(2):93.
22. De Quadros I, Gomes BP, Zaia AA, Ferraz CC, Souza- Filho FJ. Evaluation of endodontic treatments performed by students in a Brazilian Dental School. Journal of Dental Education. 2005 Oct;69(10):1161-70.
23. Benvenutti A, Scalvi M, Junior SA, Battiston C. Clinical and radiographic assessment of root canal treatments performed by dental students. RSBO Revista Sul-Brasileira de Odontologia. 2016;13(1):11-7.
24. Smith CS, Setchell DJ, Harty FJ. Factors influencing the success of conventional root canal therapy—a five-year retrospective study. International Endodontic Journal. 1993 Nov;26(6):321-33.
25. Barbakow FH, Cleaton-Jones P, Friedman D. An evaluation of 566 cases of root canal therapy in general dental practice 2. Postoperative observations. Journal of Endodontics. 1980 Mar 1;6(3):485-9.
26. Estrela C, Leles CR, Hollanda AC, Moura MS, Pécora JD. Prevalence and risk factors of apical periodontitis in endodontically treated teeth in a selected population of Brazilian adults. Brazilian Dental Journal. 2008;19(1):34- 9.
27. Azim AA, Griggs JA, Huang GJ. The Tennessee study: factors affecting treatment outcome and healing time following nonsurgical root canal treatment. International Endodontic Journal. 2016 Jan;49(1):6-16.
28. Sjögren UL, Hägglund B, Sundqvist G, Wing K. Factors affecting the long-term results of endodontic treatment. Journal of Endodontics. 1990 Oct 1;16(10):498-504.
29. Panitvisai P, Parunnit P, Sathorn C, Messer HH. Impact of a retained instrument on treatment outcome: a systematic review and meta-analysis. Journal of Endodontics. 2010 May 1;36(5):775-80.
30. Tronstad L, Asbjørnsen K, Døving L, Pedersen I, Eriksen HM. Influence of coronal restorations on the periapical health of endodontically treated teeth. Dental Traumatology. 2000 Oct;16(5):218-21.
31. Estrela C, Holland R, Estrela CR, Alencar AH, Sousa- Neto MD, Pécora JD. Characterization of successful root canal treatment. Brazilian Dental Journal. 2014 Feb;25(1):3-11.
32. Ray HA, Trope M. Periapical status of endodontically treated teeth in relation to the technical quality of the root filling and the coronal restoration. International Endodontic Journal. 1995 Jan;28(1):12-8.
33. Kojima K, Inamoto K, Nagamatsu K, Hara A, Nakata K, Morita I, et al. Success rate of endodontic treatment of teeth with vital and nonvital pulps. A meta-analysis. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology. 2004 Jan 1;97(1):95-9.
34. Heling I, Gorfil C, Slutzky H, Kopolovic K, Zalkind M, Slutzky-Goldberg I. Endodontic failure caused by inadequate restorative procedures: review and treatment recommendations. The Journal of Prosthetic Dentistry. 2002 Jun 1;87(6):674-8.
35. Saunders WP, Saunders EM, Sadiq J, Cruickshank E. Technical standard of root canal treatment in an adult Scottish sub-population. British Dental Journal. 1997 May;182(10):382-6.
36. Peak JD, Hayes SJ, Bryant ST, Dummer PM. The outcome of root canal treatment. A retrospective study within the armed forces (Royal Air Force). British Dental Journal. 2001 Feb;190(3):140-4.
37. Nair PN. On the causes of persistent apical periodontitis: a review. International Endodontic Journal. 2006 Apr;39(4):249-81.
38. Ng YL, Mann V, Gulabivala K. Tooth survival following non-surgical root canal treatment: a systematic review of the literature. International Endodontic Journal. 2010 Mar;43(3):171-89.
39. Balto H, Al Khalifah SH, Al Mugairin S, Al Deeb M, Al-Madi E. Technical quality of root fillings performed by undergraduate students in Saudi Arabia. International Endodontic Journal. 2010 Apr;43(4):292-300.
40. Moussa-Badran S, Roy B, Bessart du Parc AS, Bruyant M, Lefevre B, Maurin JC. Technical quality of root fillings performed by dental students at the dental teaching centre in Reims, France. International Endodontic Journal. 2008 Aug;41(8):679-84.