Abstract
Objective: Prevention of sexually transmitted diseases is an essential factor in managing diseases in the human population and increasing individuals’ and society’s health levels. Thus to increase our insufficient knowledge about proper prevention methods, we performed this study to assess the risk factors of the incidence of genital warts (GW).
Methods: In this case-control study, we enrolled 120 women and divided them into two groups. Sixty women with GW were set in the case group, and 60 healthy women were set in the control group. Afterwards, a questionnaire consisting of 13 questions regarding their life habituates was filled. The answers were analyzed using T-tests and chi-square test.
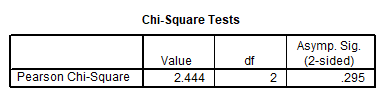
Findings: There was a statistically significant correlation between the incidence of GW and age (P-value ≤ 0.001*), the years passed from first intercourse (P-value =0.02*), and the history of venereal diseases (P-value =0.03*). However, the correlation between this disease and smoking, use of contraceptive medications, use of barrier and gravidity methods, marriage, education, the job of the individual and her partner, and the type of intercourse was not statistically significant.
Conclusion: It is interesting that although some factors may increase the risk of GW, some factors that one might reason should affect the prevalence of GW such as the use of barriers, marriage, and socioeconomics of the individuals had no significant effect on the prevalence of GW in this study.
Keywords
Genital warts, Human papillomavirus, Venereal diseases
Introduction
Human papillomaviruses (HPV) are non-enveloped, double-stranded DNA viruses responsible for the most common sexually transmitted infection worldwide [1].
Whilst there are more than 100 strains of HPV, roughly 90% of genital warts (GW) cases are due to infection with HPV types 6 and 11 [2,3].
Some types of the virus may also cause neoplastic changes and eventually result in squamous cell carcinoma [4]. Among them, HPV 16 is considered the most oncogenic, as it is accountable for roughly half of cervical cancer cases [5].
It should be noted that GWs can increase the transmission of other sexually transmitted diseases (STDs) [6-8]. Thus, proper management and prevention of infection are highly desirable.
Clinically apparent GW are seen in a small amount of the infected population, of which 90% of this population has had a history of GW. Most recent studies in different countries have shown that 5-20% of people aged between 15-40 are infected with HPV, yet only a few of them, show clinical signs of the disease [1,7].
The highest infection rate has been seen in sexually active women aged under 25. The most critical risk factor of infection with HPV is the sexual behaviour of an individual. It is noticeable that more sexual partners and more HPV-infected sexual partners may increase infection risk. External GW is highly contagious, and more than 75% of the partners of an infected individual are infected after intercourse [1,2,7].
Vaccination is an effective preventive method against HPV infection [9].
As the leading cause of cervical cancer, the burden of HPV infection is much higher in underdeveloped and developing countries. Almost 85% of worldwide deaths due to cervical cancer are recorded in these regions [10].
In the middle east, while there is a lack of data on HPV, there has been a recent increase in the number of HPV infections which could be owed to the fact that more young adults are engaging in premarital sexual affairs. Together with a slow introduction and implementation of vaccination into public health systems makes the outlook concerning [11-14].
According to studies, in Iran, the prevalence of HPV infection has increased and 9.4% of healthy women and 74% of women diagnosed with cervical cancer have an HPV infection [15-17].
Despite the lack of official statistics on vaccination rates in Iran, research has shown that the public has limited knowledge of HFPV and preventive methods such as vaccines [18,19].
As cultural and social norms affect sexual behaviour [20] and owing to insufficient data regarding risk factors associated with GW incidence in the Iranian population in Tehran, we conducted this study.
Material and Methods
The present study was an observational, analytical-descriptive, cross-sectional study on 120 women referred to the teaching hospitals of Islamic Azad University, Tehran Medical Branch between 2017 and 2020. Informed consent was obtained from all participants regarding research and publication purposes. From all the referrals, 120 women consented to participate in our study. These 120 women were divided into two groups, 60 women with GW in the case group and 60 women with no history of GW in the control group. We developed a questionnaire to collect the data from participants.
The questionnaire included 13 questions and aimed to capture participants’ demographic information, including age at the first intercourse, the number of pregnancies, protection methods if any, use of oral contraceptives (OCP), smoking status, type of intercourse (vaginal, oral, anal) and history of any venereal diseases.
Statistical analysis
SPSS Software version 26 was used for data analysis independent T-tests and chi-square test was used for data analysis a two-tailed P-value under 0.05 was considered statistically significant. The sample size of the study was calculated using the G-power application with an alpha of 0.05 and (1-β) of 0.80.
Results
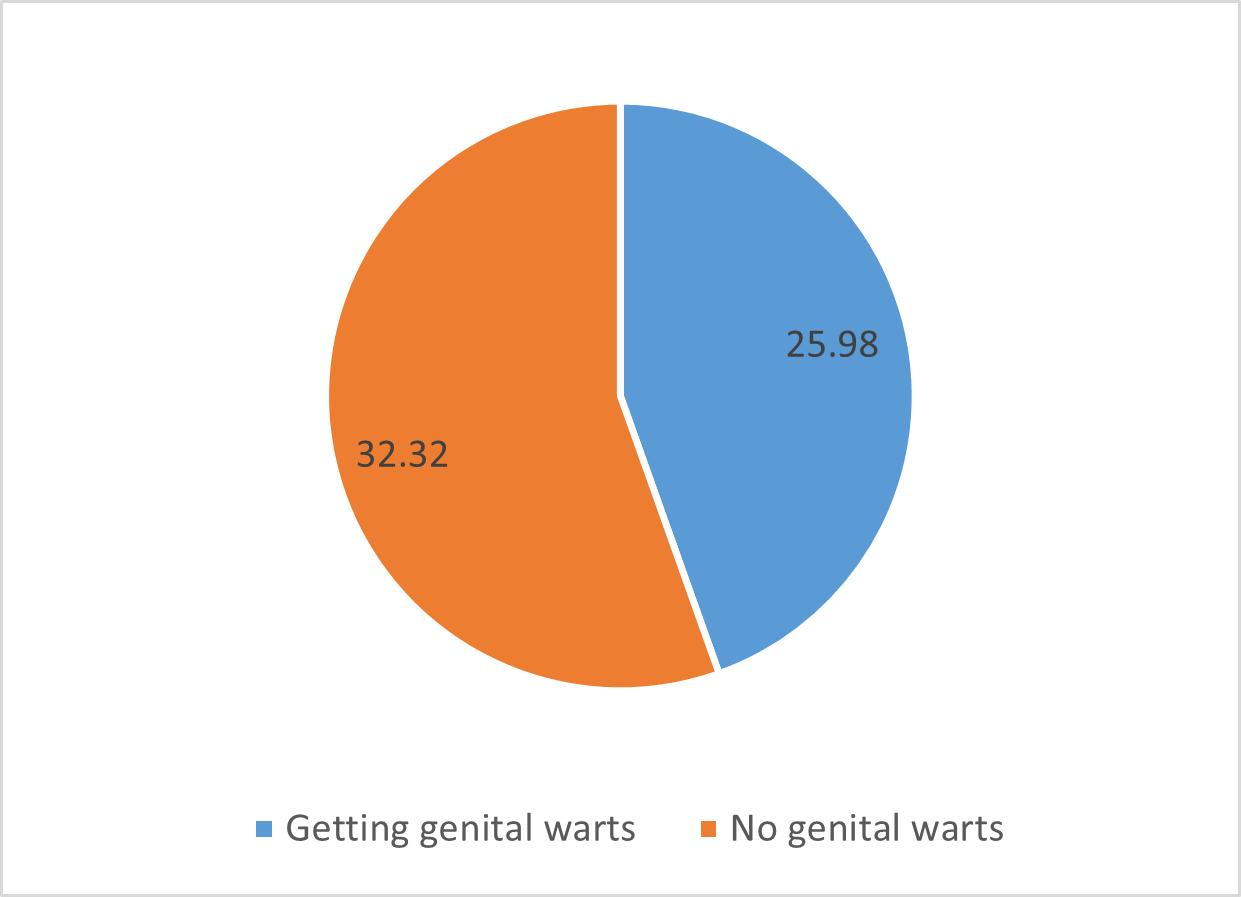
The average age of women with genital warts was 25.98 years and the average age of women without genital warts was 32.32 years (Figure 1).
Figure 1. Distribution of age frequency in the studied women based on having or not having genital warts.
75% of women with primary education, 50% of women with secondary education, and 44.4% of women with postgraduate education showed clinical signs of GW. No significant relationship was found between education level and genital warts (P>0.05) (Table 1).
Table 1. Chi-square test to investigate the relationship between education level and genital warts.
There was no significant relationship between occupation and genital warts (P>0.05).
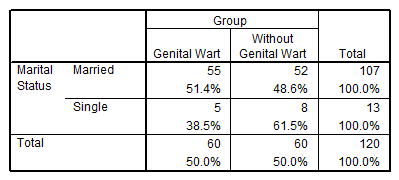
51.4% of people were married and 38.5% had genital warts. And there was no significant relationship between marital status and genital warts (p>0.05) (Table 2).
Table 2. Frequency distribution of marital status in patients and non-patients with genital warts.
59.1% of people who used OCP and 46% of those who did not use OCP had genital warts. Chi-square test showed that there was no significant relationship between OCP consumption and genital warts (P>0.05).
55.5% of people who used barrier methods and 45.7% of people who did not use barrier methods had genital warts, according to the chi-square test, there is a significant relationship between using barrier methods and having genital warts. Dari was not found (P>0.05).
Also, the presence of genital warts was more in people who smoked (53.8%). And no significant relationship was found between cigarette use and genital warts (P>0.05) (Table 3).
Table 3. Chi-square test to investigate the relationship between smoking and genital warts.
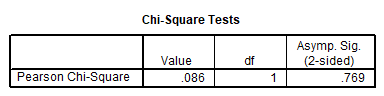
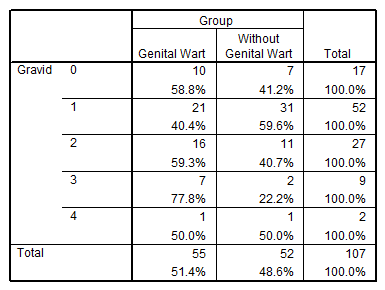
58.8% of nulli-gravid women, 40.4% of gravid 1 women, 59.3% of gravid 2 women, 77.8% of gravid 3 women and 50% of gravid 4 women had genital warts. Chi-square test showed that there was no relationship between the number of gravidity and genital warts (P>0.05) (Table 4).
Table 4. Frequency distribution of parity number in studied women based on genital warts.
In the frequency distribution of parity number in the studied women based on having genital warts, 66.7% of women with parity 3 had genital warts and no significant relationship was found between parity number and having genital warts.
59.1% of people taking OCP had genital warts. No significant relationship was found between OCP consumption and genital warts (P>0.05).
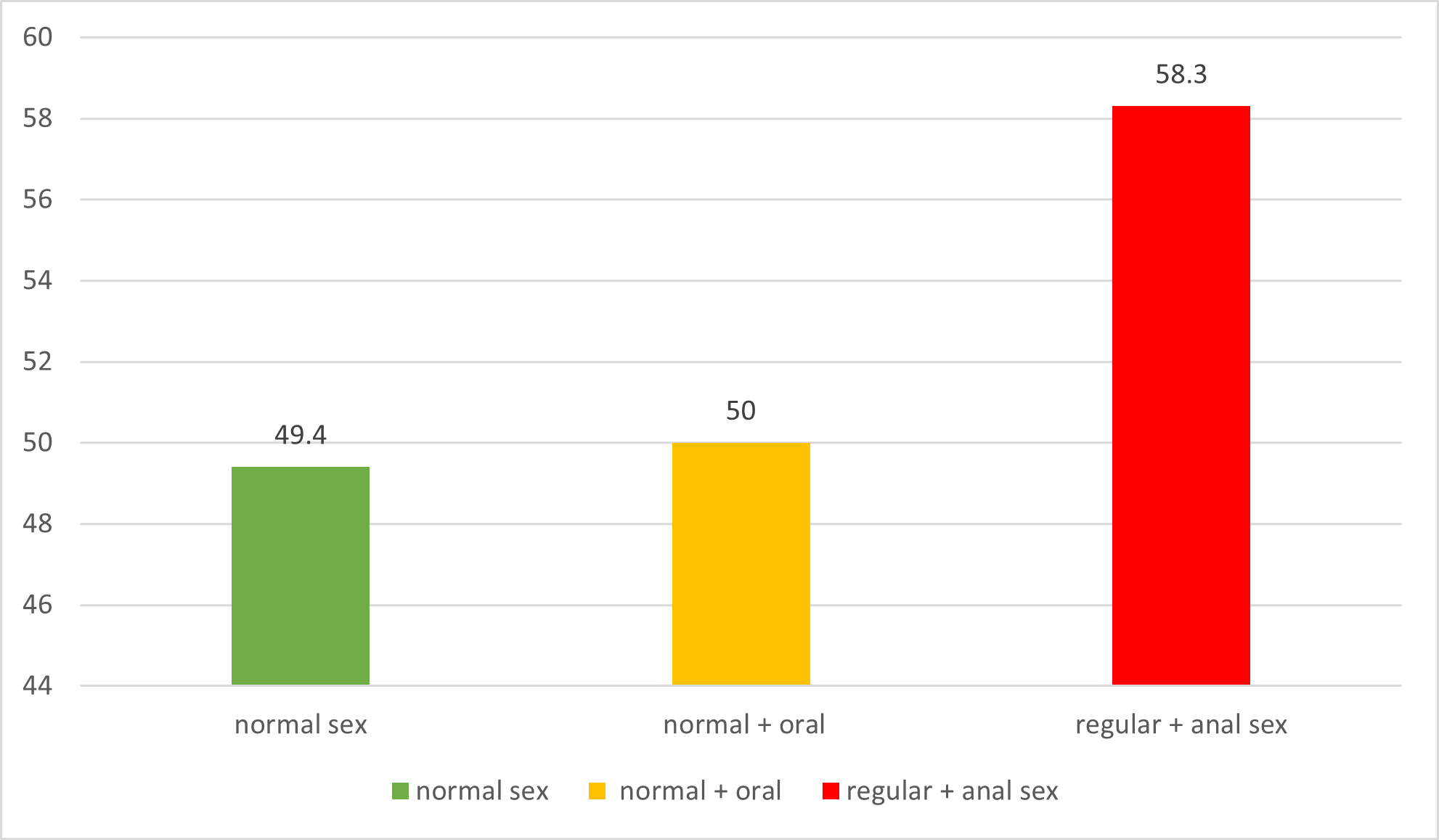
49.4% of people who have normal sex, 50% of people who have normal + oral sex and 58.3% of people who had regular + anal sex had genital warts (Figure 2).
Figure 2. Frequency distribution of sexual habit type in the studied women based on genital warts.
Discussion and Conclusion
In this study, a significant correlation between the incidence of GW and age, the time of the first intercourse, and a positive history of venereal diseases were noted.
Further, our study results showed that the recovery rate in elderly patients is lower, and they need more treatment sessions. The recurrence rate for married and multi-partner women is significantly higher than the others. The age of patients and the size of the lesions greatly influence the recovery rate, and the critical risk factors for the recurrence of the disease are insecure sexual contact during treatment and after the treatment period.
It is interesting that although education level, use of protection, and socioeconomic status might be potential factors in the prevalence of GW and thus other STDs, in this study no significant correlation between such factors and the incidence of GWs was observed. Thus, we suspect that regardless of socioeconomics, or sexual behaviour and use of protection, women should be vaccinated against HPV before engaging in sexual activity. Nonetheless, to further evaluate the effects of the aforementioned factors and the incidence of GWs and thus, other STDs more studies with greater populations are needed.
Lastly, according to the present study results and compared with the results of other studies, it was concluded that the risk of incidence of genital wart is increased with age, an increase of the time passed from the first intercourse, and the existence of a history of venereal diseases, due to adverse effect of these lesions on the quality of life of an individual and increasing the rate of the necessity of cesarian section.
Recent studies have described the importance of comprehensive sexual education for women in Iran and the need for wider and adequate distribution of the HPV vaccine in Iran [21,22]. It is important to note that our sample size primarily consists of women who lived in the vicinity of the capital city. This study did not capture women who live in regional and rural areas of Iran and future studies should consider a broader sample size for further evaluation.
Declarations
Ethics approval and consent to participate
After the evaluation and acceptance of this study by the ethics committee of the Islamic Azad University, Tehran Medical Branch, the study was explained to the participants. Informed consent was obtained from all participants prior to the commencement of the study. The participants were assured that their personal information would not be shared with any individual or organization. The experimental protocols were approved by the Islamic Azad University, Tehran Medical Branch ethics committee. This study was performed in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on request.
Competing interests
The authors declare that they have no competing interests.
Funding
Not applicable (no funds were received).
Authors' contributions
A.L. and S.T.N. conceptualised the project and developed the questionnaire, conducted data analysis, drafted the manuscript, and performed the literature review.
Acknowledgments
We thank all the participants for their cooperation in this project. We would like to thank Mr Benyamin Hakak-Zargar and Mr Arad Solgi for conducting thorough editing of the manuscript.
References
2. Faridi R, Zahra A, Khan K, Idrees M. Oncogenic potential of Human Papillomavirus (HPV) and its relation with cervical cancer. Virol J. 2011 Jun;8:269.
3. Braaten KP, Laufer MR. Human Papillomavirus (HPV), HPV-Related Disease, and the HPV Vaccine. Rev Obstet Gynecol. 2008;1(1):2-10.
4. Muñoz N, Bosch FX, de Sanjosé S, Herrero R, Castellsagué X, Shah K V, et al. Epidemiologic classification of human papillomavirus types associated with cervical cancer. N Engl J Med. 2003 Feb;348(6):518-27.
5. Clifford GM, Smith JS, Aguado T, Franceschi S. Comparison of HPV type distribution in high-grade cervical lesions and cervical cancer: a meta-analysis. Br J Cancer. 2003 Jul;89(1):101-5.
6. Ferreira Costa AP, dos Santos MG, Oliveira Cobucci RN. Sexually transmitted co-infections in persons living with HIV. Frontiers in Clinical Drug Research - HIV. 2019;2019:138-52.
7. Cubie HA. Diseases associated with human papillomavirus infection. Virology. 2013 Oct;445(1-2):21-34.
8. Paba P, Bonifacio D, Di Bonito L, Ombres D, Favalli C, Syrjänen K, et al. Co-expression of HSV2 and Chlamydia trachomatis in HPV-positive cervical cancer and cervical intraepithelial neoplasia lesions is associated with aberrations in key intracellular pathways. Intervirology. 2008;51(4):230-4.
9. Dilley S, Miller KM, Huh WK. Human papillomavirus vaccination: Ongoing challenges and future directions. Gynecol Oncol. 2020 Feb;156(2):498-502.
10. Small WJ, Bacon MA, Bajaj A, Chuang LT, Fisher BJ, Harkenrider MM, et al. Cervical cancer: A global health crisis. Cancer. 2017 Jul;123(13):2404-12.
11. Obeid DA, Almatrrouk SA, Alfageeh MB, Al-Ahdal MNA, Alhamlan FS. Human papillomavirus epidemiology in populations with normal or abnormal cervical cytology or cervical cancer in the Middle East and North Africa: A systematic review and meta-analysis. J Infect Public Health. 2020 Sep;13(9):1304-13.
12. Jumaan AO, Ghanem S, Taher J, Braikat M, Al Awaidy S, Dbaibo GS. Prospects and challenges in the introduction of human papillomavirus vaccines in the extended Middle East and North Africa region. Vaccine. 2013 Dec;31 Suppl 6:G58-64.
13. DeJong J, Jawad R, Mortagy I, Shepard B. The sexual and reproductive health of young people in the Arab countries and Iran. Reprod Health Matters. 2005 May;13(25):49-59.
14. Castle PE, Maza M. Prophylactic HPV vaccination: past, present, and future. Epidemiol Infect. 2016 Feb;144(3):449-68.
15. Jamdar F, Farzaneh F, Navidpour F, Younesi S, Balvayeh P, Hosseini M, et al. Prevalence of human papillomavirus infection among Iranian women using COBAS HPV DNA testing. Infect Agent Cancer. 2018;13:6.
16. Malary M, Moosazadeh M, Hamzehgardeshi Z, Afshari M, Moghaddasifar I, Afsharimoghaddam A. The Prevalence of Cervical Human Papillomavirus Infection and the Most At-risk Genotypes Among Iranian Healthy Women: A Systematic Review and Meta-analysis. Int J Prev Med. 2016;7:70.
17. Jalilvand S, Shoja Z, Hamkar R. Human papillomavirus burden in different cancers in Iran: a systematic assessment. Asian Pac J Cancer Prev. 2014;15(17):7029-35.
18. Bruni L, Albero G, Serrano B, Mena M, Collado JJ, Gómez D, et al. ICO/IARC Information Centre on HPV and Cancer (HPV Information Centre). Human Papillomavirusand Related Diseases in Iran (Islamic Republic of). Summary Report 22 October 2021.
19. Taebi M, Riazi H, Keshavarz Z, Afrakhteh M. Knowledge and Attitude Toward Human Papillomavirus and HPV Vaccination in Iranian Population: A Systematic Review. Asian Pac J Cancer Prev. 2019 Jul;20(7):1945-9.
20. Singer MC, Erickson PI, Badiane L, Diaz R, Ortiz D, Abraham T, et al. Syndemics, sex and the city: understanding sexually transmitted diseases in social and cultural context. Soc Sci Med. 2006 Oct;63(8):2010-21.
21. Shahsavari S, Alavi A, Razmjoue P, Mohseni S, Ranae V, Hosseini Z, et al. A predictive model of GW preventive behaviors among women in the south of Iran: application of health belief model. BMC Womens Health. 2022 Mar;22(1):63.
22. Mohammadpour F, Mansouri A, Hadjibabaie M. Utilization Evaluation of Human Papilloma Virus Vaccine (GARDASIL®) in Iran; A Cross-Sectional Study. Iran J Pharm Res IJPR. 2020;19(1):68-76.