Abstract
Background: Developmental dislocation of the patella (DDP) is rare in humans but common in dogs. The canine syndrome, termed patellar luxation (PL), is an inherited condition related to genetic selection of dogs with conformational defects. Breeds with short, bowed legs, including chihuahuas, toy poodles, and bull terriers are predisposed to medial patellar luxation (MPL). Dogs with occult MPL have abnormal patellar tracking but don’t experience visible lameness or exercise intolerance. Management of occult MPL is influenced by the risks and costs of surgical intervention versus the potential risks and costs of avoiding surgery.
Objective: To determine the risk of long-term lameness and the rate of subsequent surgery in dogs with occult grade II MPL.
Method: We performed a retrospective dog owner survey and reviewed the clinical records of adult dogs diagnosed with occult grade II MPL. We included asymptomatic dogs managed non-surgically, with a minimum of 4-years’ follow-up. We used clinical records and owner questionnaires to identify dogs who developed clinically-relevant lameness on a previously asymptomatic limb.
Results: Thirty-eight dogs were included, with an average follow-up of 4.25-years. Seventeen dogs returned for unscheduled MPL surgery at an average of 15 months after initial presentation. A further two dogs developed chronic lameness which was not managed surgically.
Conclusion: Fifty percent of adult dogs with occult grade II MPL developed chronic lameness or required surgery.
Introduction
Veterinary healthcare follows the same guiding principle as human healthcare. Namely, veterinarians, like doctors, must do no harm. Avoiding unnecessary harm is more difficult if a treatment is preventative rather than therapeutic. Justifying surgical treatment is especially challenging if a disease isn’t clinically important at the time of diagnosis. Many developmental veterinary conditions can present without clinical signs [1]. These so-called occult conditions pose a dilemma for veterinary surgeons and pet owners. Performing prophylactic surgery means accepting the morbidity, risk, and cost of an operation which might be unnecessary. Veterinarians regularly face this dilemma because prophylactic neutering operations are routine practice. For instance, laparoscopic ovariectomy is a low-morbidity operation performed to eliminate or reduce the risk of potentially life-threatening conditions including uterine infection and mammary cancer [2].
Developmental dislocation of the patella (DDP) is rare in humans but common in dogs. The canine syndrome, termed patellar luxation (PL), is an inherited condition. Prevalence is increasing over time because of the growing popularity of dog breeds with short, bowed limbs (Figure 1).

Figure 1. Volume-reconstructed CT scan of a French bulldog’s pelvic limbs showing typical femoral bowing, tibial torsion, patella alta and left-sided medial patellar luxation (MPL).
Although there is no current consensus on the exact pathogenesis of canine PL, a popular hypothesis states that the problem begins in the hip [3]. Puppies with MPL have a medially displaced quadriceps origin, coxa vara, and decreased femoral neck anteversion. Medially displaced muscular forces cause medial bowing and rotation of the growing distal femur and proximal tibia (Figure 2). If early diagnosis is possible, there’s a compelling argument for surgical intervention. Surgery in puppies has the potential to mitigate the severe limb deformities which can develop with continued growth [4]. In contrast, ideal management of occult PL in adults is controversial. The decision to intervene depends on the risks and costs of surgery weighed against the potential risks and costs of avoiding surgery.
Figure 2 shows the standard I-IV grading system for medial patellar luxation (MPL), which is the commonest form of developmental canine PL. A relationship between MPL grade and clinical importance is well accepted. In grade I MPL, the patella doesn’t spontaneously dislocate, so surgery isn't indicated. In contrast, grades III and IV MPL consistently cause lameness, so surgical treatment is justifiable [6]. Controversy surrounds the best management of grade II MPL. This grade covers a broad spectrum of clinical relevance. Some dogs demonstrate frequent or constant lameness, while others have infrequent lameness or no lameness at all. Consequently, for adult dogs with grade II MPL, the decision to operate is usually made based on the frequency of lameness episodes. For example, lameness occurring once every year would be managed non-surgically, while constant lameness would be managed surgically. As MPL is caused by abnormal conformation, veterinary surgeons often diagnose dogs with bilateral MPL. Many dogs with bilateral MPL are only lame on one hindlimb. A decision to treat occult MPL in the opposite knee might be justifiable. Surgeons can rationalize that simultaneous bilateral surgery subjects their patient to a single episode of surgical rehabilitation instead of two. Critically, this argument is only valid if progression from occult MPL to clinically significant MPL is likely.
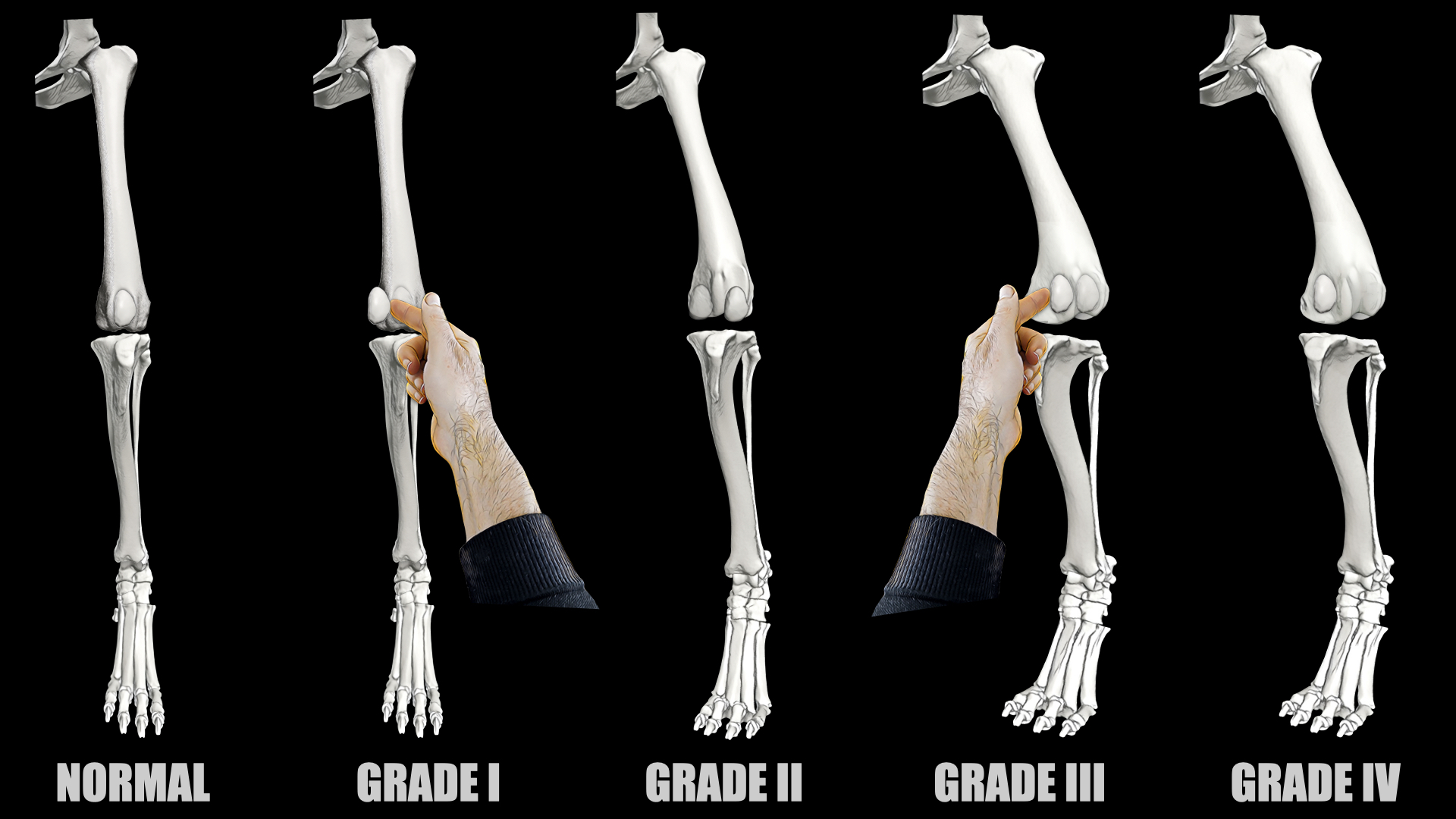
Figure 2. The four grades of medial dislocation of the canine patella, also known as medial patellar luxation (MPL) [5]. Grade I: The patella can be manually dislocated but returns to a normal position when released. Affected dogs are not lame. Grade II: The patella dislocates spontaneously when the knee is flexed or extended. Reduction is possible by extending the knee or applying lateral pressure to the patella. A torsional deformity of the tibia is typical. Some dogs with grade II patellar luxation are lame and some aren’t. Grade III: The patella is permanently dislocated but can be manually reduced. It spontaneously dislocates if lateral pressure is released. Severe bony deformities are typical. Grade IV: The patella is permanently dislocated and cannot be reduced.
If sufficient outcome data are available, a valuable epidemiological metric is the number-needed-to-treat (NNT). While NNT has been used in veterinary medicine in the past, its use is uncommon [7]. To calculate the NNT for occult canine MPL, a sample population of affected dogs would need to be followed for a predetermined duration, and the proportion of dogs suffering an adverse outcome would need to be established during that time. As canine MPL is significantly more prevalent than lateral PL [8], we performed this study using a sample population of dogs affected by occult grade II MPL.
Methods
We performed a retrospective cohort survey. Our inclusion criteria were:
All dogs were skeletally mature; i.e. >12-months-old at the time of diagnosis.
Unilateral MPL surgery was performed at one of three specialist referral centres.
Occult grade II MPL was diagnosed in the opposite (non-surgical) knee. A specialist or resident-in-training confirmed the diagnosis using the standard grading system (Figure 2) [5]. "Occult" MPL was defined as no previous or current lameness and absence of knee pain during the veterinary assessment.
At least 4-years’ follow-up. If unscheduled contralateral MPL surgery was performed, we defined follow-up duration as the time elapsed between initial presentation and contralateral surgery.
We excluded dogs with concurrent knee pathology (e.g. ACL injury) or prior hindlimb surgery. Dogs were excluded if their surgeon had pre-planned staged contralateral MPL surgery. We excluded dogs with incomplete records, equivocal grading, or grading using an alternative system. We retrieved the following data from the clinical records: (1) Age at initial presentation; (2) surgically treated limb; (3) breed; (4) bodyweight; and (5) gender. We defined an adverse outcome as subsequent contralateral MPL surgery or clinically-important lameness. This was defined as lameness occurring at least once every month or chronic lameness that prompted surgical intervention. If the clinical notes didn't document an adverse outcome, we contacted the dog’s owners by telephone. We asked them to complete a questionnaire designed to establish whether lameness occurred on the previously asymptomatic limb. We categorized lameness according to frequency; i.e. constant lameness, lameness at least once per week, once per month, or once per year. We asked if owners were treating lameness with medication and if they were restricting exercise.
Results were grouped based on outcome (Figures 3A and 3B). Statistical analysis was performed using statistical software (IBM SPSS v19, August 2010, SPSS, Armonk, NY). The Kolmogorov-Smirnov test was used for evaluation of normality of continuous variables (i.e. age, weight, time to last follow-up and surgery). Results were expressed as mean ± standard deviation (SD) for normally distributed variables and median for non-normally distributed variables. All variables except weight followed a normal distribution. The NNT is the number of patients needed to treat to prevent one adverse outcome.
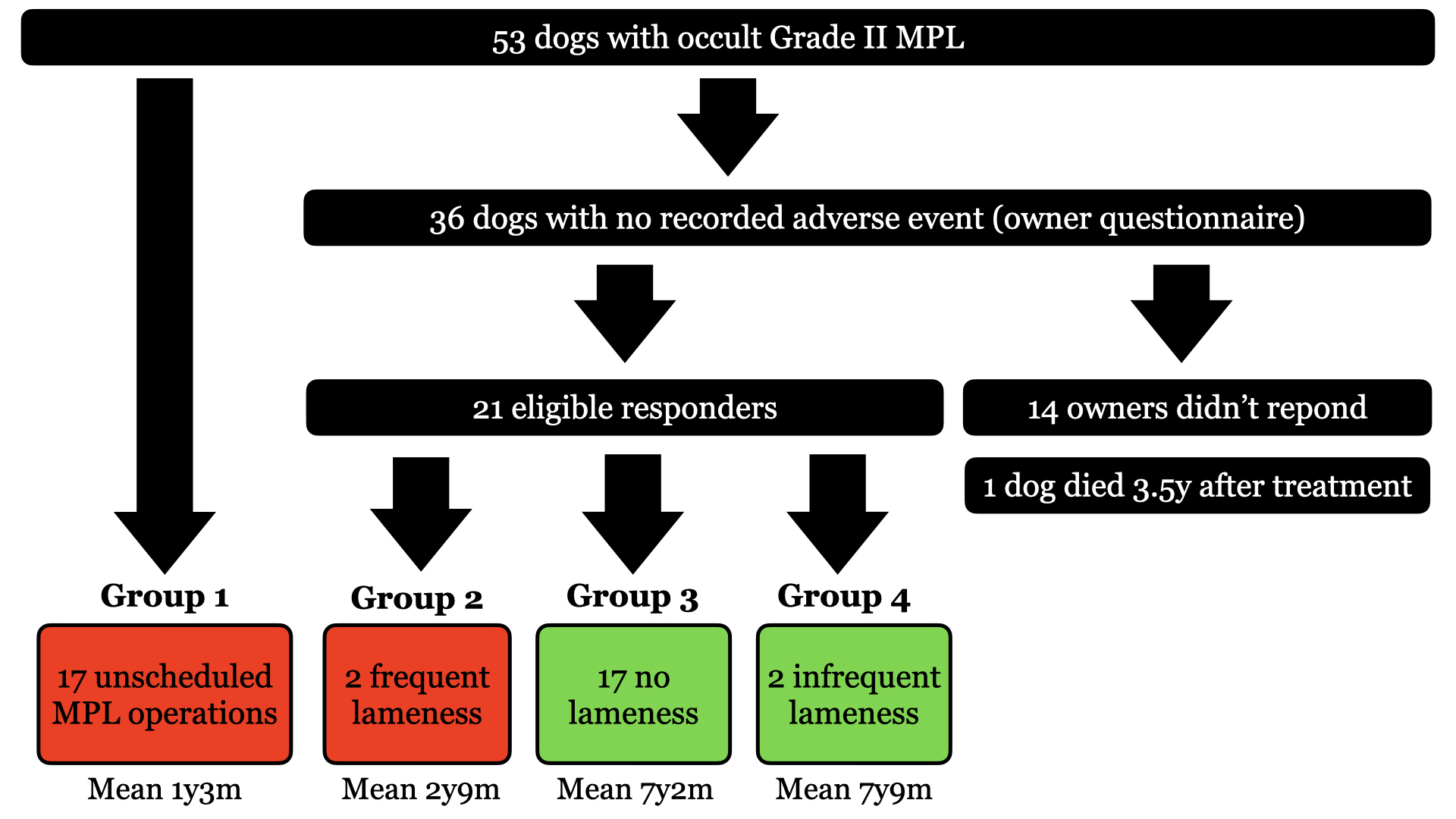
Figures 3A and B Group 1. Unscheduled contralateral MPL surgery. Group 2: Clinically-important contralateral lameness that would justify surgical treatment. Group 3: No reported long-term lameness. Group 4: Infrequent contralateral lameness.
Results
Results are summarized in Figure 3. Mean age at initial presentation was 30 months (SD 24 months) and median bodyweight was 8.6 kg (range 1.8-56 kg). There were 18 males (12 neutered) and 20 females (14 neutered). We identified 53 dogs with occult grade II MPL. Seventeen of these dogs returned to the same institution for unscheduled contralateral MPL surgery. Of the 36 owners of dogs who didn't return, 22 responded to our questionnaire. We excluded one dog due to inadequate follow-up because he'd died 43 months after surgery.
According to our pre-determined criteria, groups 1 and 2 suffered an adverse event. Group 1 included 17 dogs who had unscheduled contralateral MPL surgery. Mean time between the initial and contralateral surgery was 1 year 3 months (SD 1 year 11 months). Group 2 included two dogs who suffered clinically-important contralateral lameness attributed to MPL. These two dogs were surgical candidates, but surgery was not performed for financial reasons. One of these dogs received intermittent non-steroidal anti-inflammatory medication. Mean time between the initial surgery and contralateral lameness onset was 2 years 9 months (SD 3 years 5 months).
Groups 3 and 4 didn’t suffer an adverse event. Group 3 included 17 dogs with no history of lameness. Follow-up duration was the time elapsed until the questionnaire or until the date of the dog's death. Mean follow-up was 7 years 2 months (SD 2 years 5 months). Group 4 included 2 dogs with lameness occurring on average once per year. In both cases, lameness spontaneously resolved without veterinary intervention. Mean follow-up was 7 years 9 months (SD 2 years 6 months).
According to our predetermined criteria, an adverse event occurred in 19/38 cases; i.e. in 50% of dogs, with a mean follow-up of 4 years 3 months. Thus, if bilateral surgery had been performed in the first instance, 1/2 dogs would have endured an unnecessary contralateral operation (i.e. the NNT was two).
Discussion
Surgery on a pet involves separation from their owners, surgical aftercare, risk, and financial cost. Veterinary surgeons have access to excellent painkillers, but there will always be some discomfort. We have very safe anesthetic and surgical protocols, but there will always be some risk. For occult MPL, owners must balance these risks against the risk of avoiding surgery. This study aimed to establish the natural history of asymptomatic patellar luxation. Knowing the likelihood an occult problem will progress to a clinically-important problem is valuable. Our data allows dog carers to decide if surgical morbidity, cost, and risk are justifiable. We showed that 50% of adult dogs with occult grade II MPL suffer an adverse long-term outcome. In effect, for every two "preventative" operations, one dog is spared an adverse outcome, whilst another must endure an unnecessary procedure.
Our data has value in counselling owners of affected dogs, but it should be presented as an estimate. The selection of dogs who had already undergone surgery is a potential source of bias. It's possible that dog owners might have been more inclined to choose surgery on the opposite knee if the result of the first operation was good. This bias might be amplified if owners believed that avoiding surgery would pose a high risk of future problems. It's also possible that the attending surgeon might have warned owners of a possible adverse effect of avoiding surgery without recording their advice in the medical record. This potential source of bias would have caused a reduction in the estimated NNT.
Another possible source of bias is diagnostic misinterpretation. Lameness affecting the opposite limb might have been missed, although this seems unlikely. In all cases, owners reported an intermittent or constant limp on the limb which was originally managed surgically. It's fair to assume that these same owners should have been equally capable of detecting limping on the opposite hindlimb. It could be argued that severe ipsilateral lameness might have obscured contralateral lameness. However, in this scenario we would have expected contralateral lameness to manifest soon after surgical correction of the severely affected limb. Nevertheless, we acknowledge that this potential bias is possible in the five dogs that re-presented less than 3 months after initial surgery. The average length of time to contralateral surgery in the remaining dogs was 15 months.
Another possible source of bias is the intentional exclusion of puppies and adult dogs with grades I, III and IV MPL. We excluded immature animals due to the potential for progressive limb deformity associated with continued growth. This, in turn, could increase the severity of MPL [4]. Consequently, it's likely that including these cases would have increased the likelihood of an adverse outcome. We didn't include occult grade I MPL in our analysis because this grade doesn't carry a surgical indication. Thus, we wouldn't expect veterinary professionals to warn owners of adult dogs with grade I MPL that future surgery is likely. Nevertheless, it remains possible that some dogs with grade I MPL might progress to a higher grade of clinically-important MPL later in life. In addition, some dogs with bilateral grade III or IV MPL might not limp because they’re equally lame on the left and right hindlimb. Although it was not our intention to assess these groups, this may be an interesting area of future research.
Fundamentally, NNT is a metric used to estimate the relative risks of performing an intervention compared with not performing the intervention. Consequently, the ideal study of occult grade II MPL would involve prospective comparison of a group of dogs having “prophylactic” MPL surgery and a control group managed non-surgically. Possible confounding variables would be controlled. These include exercise, diet and body condition. Surgical adverse effects (i.e. complications and financial costs) would be compared to the adverse outcomes of the control group. Although this analysis was beyond the scope of our study, others have assessed the relative complication rates of simultaneous bilateral MPL repair, unilateral MPL repair and staged bilateral MPL repair [9,10]. In these studies, the overall complication rates were higher in dogs having simultaneous surgery on both knees, although differences were not statistically significant. Even so, MPL surgery complications are an important consideration, with quoted ranges from 18 to 43% [9-14]. Major complications that trigger surgical revision are reported in 7 to 18% of operated dogs [9-13]. Previous studies have not specifically addressed the more subjective problem of early postoperative pain and disability. Intuitively, increased discomfort and limited mobility are expected after simultaneous surgery on both hind limbs.
An adverse effect which we didn’t encounter in our study is degenerative ACL injury. A potential relationship between untreated MPL and ACL injury has been proposed [14,15]; however, a statistical relationship was only demonstrated in dogs with grade IV MPL [16]. In our study, none of the dogs managed surgically had any evidence of current ACL injury. Although the ACL is routinely inspected during MPL repair, we accept the possibility that microscopic disease was missed in some cases.
In conclusion, animal carers have a right to make informed choices for their pets. Owners of dogs with occult MPL face a dilemma, but the data provided in this study should make it easier to solve. Owners of affected dogs will be asked, "How much future risk is worth your pet enduring surgery on both knees instead of one knee?” In this study, we showed these carers that future risk is ~50%.
Conflict of Interest
The author has no financial or personal relationship with other people or organizations that could influence or bias the content of this review article.
References
2. Jitpean S, Hagman R, Ström Holst B, Höglund OV, Pettersson A, Egenvall A. Breed variations in the incidence of pyometra and mammary tumours in Swedish dogs. Reproduction in Domestic Animals. 2012 Dec;47:347-50.
3. Roush JK. Canine patellar luxation. Veterinary Clinics of North America: Small Animal Practice. 1993 Jul 1;23(4):855-68.
4. Fossum T. Small animal surgery (3rd). St. Louis, MO: Mosby Elsevier; 2007.
5. Putnam RW. Patellar Luxation in the Dog. (Thesis). University of Guelph. 1968; 761281039.
6. Johnston SA, Tobias KM. Veterinary surgery: small animal expert consult-E-book. Elsevier Health Sciences; 2017 Jun 14.
7. Imhoff DJ, Gordon-Evans WJ, Evans RB, Johnson AL, Griffon DJ, Swanson KS. Evaluation of S-adenosyl l-methionine in a double-blinded, randomized, placebo-controlled, clinical trial for treatment of presumptive osteoarthritis in the dog. Veterinary Surgery. 2011 Feb;40(2):228-32.
8. O’Neill DG, Meeson RL, Sheridan A, Church DB, Brodbelt DC. The epidemiology of patellar luxation in dogs attending primary-care veterinary practices in England. Canine Genetics and Epidemiology. 2016 Dec;3(1):1-2.
9. Clerfond P, Huneault L, Dupuis J, Moreau M, Auger J. Unilateral or single-session bilateral surgery for correction of medial patellar luxation in small dogs: short and long-term outcomes. Veterinary and Comparative Orthopaedics and Traumatology. 2014;27(06):484-90.
10. Fullagar BA, Rajala-Schultz P, Hettlich BF. Comparison of complication rates of unilateral, staged bilateral, and single-session bilateral surgery for the treatment of bilateral medial patellar luxation in dogs. The Canadian Veterinary Journal. 2017 Jan;58(1):39.
11. Alam MR, Lee JI, Kang HS, Kim IS, Park SY, Lee KC, et al. Frequency and distribution of patellar luxation in dogs. Veterinary and Comparative Orthopaedics and Traumatology. 2007;20(01):59-64.
12. Cashmore RG, Havlicek M, Perkins NR, James DR, Fearnside SM, Marchevsky AM, et al. Major complications and risk factors associated with surgical correction of congenital medial patellar luxation in 124 dogs. Veterinary and Comparative Orthopaedics and Traumatology. 2014;27(04):263-70.
13. Gibbons SE, Macias C, Tonzing MA, Pinchbeck GL, McKee WM. Patellar luxation in 70 large breed dogs. Journal Of Small Animal Practice. 2006 Jan;47(1):3-9.
14. DeAngelis M. Patellar luxation in dogs. The Veterinary Clinics of North America. 1971 Sep;1(3):403-15.
15. Slatter DH, editor. Textbook of small animal surgery. Elsevier Health Sciences; 2003.
16. Campbell CA, Horstman CL, Mason DR, Evans RB. Severity of patellar luxation and frequency of concomitant cranial cruciate ligament rupture in dogs: 162 cases (2004-2007). Journal of the American Veterinary Medical Association. 2010 Apr 15;236(8):887-91.
