Abstract
We described a 15-year-old- a boy who presented with neurofibromatosis type 1 and Crohn’s disease. Neurofibromatosis 1 (NF1) is the most common form of NF, affecting 1 in 3000 individuals. Crohn’s disease is one of the inflammatory bowel diseases. Its incidence is significantly rising in Ireland. Concomitant association of NF1 and Crohn’s disease is a rare finding. This is the first case reported in the paediatric population.
Keywords
Neurofibromatosis type1, Crohn’s disease
Abbreviations
NF1: Neurofibromatosis type1; CD: Crohn's Disease
Introduction
Neurofibromatosis 1 (NF1) is the most common form of NF, affecting 1 in 3000 individuals. Crohn’s disease (CD) is one of the inflammatory bowel diseases, its incidence is significantly rising in Ireland [1]. Concomitant association of NF1 and CD is a rare finding, this is the first case reported in the pediatric population.
Case Report
A 14-year-old boy was referred to the pediatric gastroenterology team with a 3-month history of recurrent episodes of moderate to severe abdominal pain, unrelated to mealtime and occasionally waking him from sleep. He had tenesmus and urgency, as well as blood in the stool. He had lost 1.5 kg over 2 months. There was no family history of gastrointestinal disease. There was no history of mouth ulcers. He denied any recent dietary changes, illnesses, or travel. NF type 1 was diagnosed at 1 year of age. He had two large plexiform neurofibromas which required 2 previous debulking procedures, 4 years apart. He was on MEK inhibitor (Selumetinib) for 2 years, this had been recently stopped as it has a known association with colitis [2].
On physical examination, he had multiple neurofibromas, axillary freckling and café au lait spots with plexiform neurofibromata on the left upper lip and right medial foot. Abdominal examination revealed left iliac fossa tenderness. He had inflamed peri-anal skin tags and fissures.
Full blood count, renal function, liver function and stool for microbiology, were all reported as normal for age, however, the inflammatory markers were moderately elevated with an erythrocyte sedimentation rate of 42 mm per hour and C-reactive protein of 41. Stool calprotectin was significantly elevated on two occasions, 1946 and 1972.
Oesophagogastroduodenoscopy and ileocolonoscopy were performed which revealed scattered aphthae throughout the colon (Figure 1).
Figure 1. Scattered aphthae throughout colon.
Histology revealed focal granulomatous inflammation of the duodenal cap and patchy chronic colitis with multifocal giant cells, consistent with CD (Figures 2 and 3).
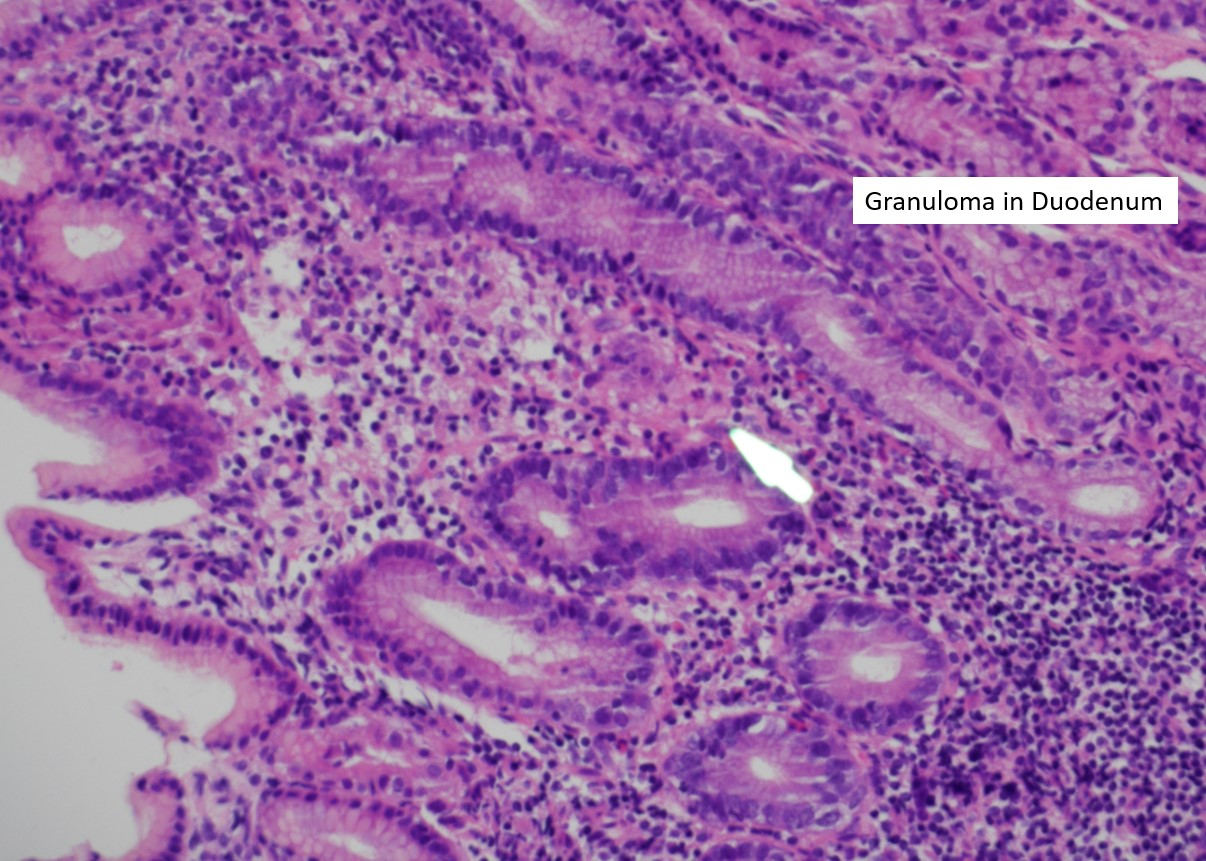
Figure 2. Granuloma in the Duodenum.

Figure 3. Giant cell in rectum.
He is now doing well on treatment with anti TNF (Infliximab). He is due to meet with his NF team to discuss restarting MEK inhibitor (Selumetinib) to treat his Plexiform neuromas.
Discussion
NF1 is an autosomal dominant genetic condition secondary to a mutation on chromosome 17q. The protein involved is neurofibromin, which participates in the Ras signaling pathway, functioning as a tumor suppressor. The gastrointestinal complications of NF1 include constipation, gastrointestinal neurofibromas, or schwannomas, bleeding, bowel obstruction, and rarely, gastrointestinal stromal tumors [3].
Pediatric inflammatory bowel disease (IBD) results in chronic inflammation of the gastrointestinal tract, and occasionally other organs. IBD can cause symptoms such as abdominal pain, bloody diarrhea, fatigue, weight loss, and malnutrition and negatively impacts the quality of life. The two main subtypes are ulcerative colitis and CD. CD has a different pattern of chronic inflammation that extends beyond the lining of the intestine, potentially affecting any segment of the intestine from the mouth to the anus. Our patient also has perianal CD.
The incidence of IBD is rapidly rising [4]. So far, no common pathway was contemplated for NF1 and CD, however, both have genetic speculation.
Selumetinib, a MEK inhibitor, is a biologic agent recently approved for the treatment of inoperable plexiform neurofibromas in patients with NF1. The most common toxic effects are grade 1 and 2 gastrointestinal symptoms (nausea, vomiting, or diarrhea) [5]. Perforation, colitis, ileus, and intestinal obstruction occurred in adult patients receiving MEK inhibitors (Selumetanib); however, these complications were absent in pediatric patients enrolled in the SPRINT trial [2].
In our patient, it was initially thought that his symptoms may have been caused by Selumetanib so the medication was stopped.
There are two reported cases of NF1 and Ulcerative Colitis in pediatrics [6,7]. To our knowledge this is the first case report of NF1 and CD in the pediatric population.
References
2. Anderson MK, Johnson M, Thornburg L, Halford Z. A Review of Selumetinib in the Treatment of Neurofibromatosis Type 1–Related Plexiform Neurofibromas. Annals of Pharmacotherapy. 2022 Jun;56(6):716-26.
3. Lehan E, Wang T, Soboleski D, Acker A, Kehar M. Inflammatory Bowel Disease and Primary Sclerosing Cholangitis in a Pediatric Patient With Neurofibromatosis Type 1. ACG Case Reports Journal. 2021 May;8(5).
4. S. Hussey et al. DOCHAS: Continuing to create hope for children with Inflammatory Bowel Disease. National Children's Research Centre. 06/02/2022. https://www.nationalchildrensresearchcentre.ie/our_impact/dochas-continuing-to-create-hope-for-children-with-inflammatory-bowel-disease
5. Gross AM, Wolters PL, Dombi E, Baldwin A, Whitcomb P, Fisher MJ, et al. Selumetinib in Children with Inoperable Plexiform Neurofibromas. The New England Journal of Medicine. 2020 Apr 9;382(15):1430-42.
6. Adams W, Mitchell L, Candelaria-Santiago R, Hefner J, Gramling J. Concurrent ulcerative colitis and neurofibromatosis type 1: the question of a common pathway. Pediatrics. 2016 Feb 1;137(2).
7. Baratelli F, Le M, Gershman GB, French SW. Do mast cells play a pathogenetic role in neurofibromatosis type 1 and ulcerative colitis?. Experimental and Molecular Pathology. 2014 Apr 1;96(2):230-4.
