Short Communication
If there are many ways of performing the same operation, it means that none of these are quite right.
- Livio Zava, General Surgeon, Treviso, Italy, 1967.
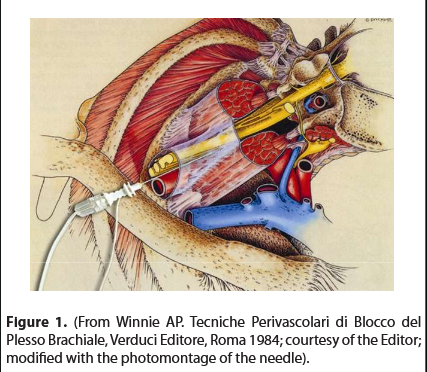
In the last century, starting from 1911 (Kulenkampff) [1], more than twenty upper limb blocking techniques had been described, each of these blocks with its owns strengths and weaknesses (complications). Personally, in the early 80s I still applied Kulenkampff’s supraclavicular technique modified by Moore [2]; in one week I had had two pneumothorax complications. I had then adopted Winnie’s interscalene block [3] and for some time the results were satisfactory. In 1985, applying Winnie’s technique for shoulder surgery, once the desired paraesthesia was evoked, aspirating, before injecting the anesthetic test bolus (2 ml), a thin trace of blood appeared in the syringe, which I had optimistically attributed to a broken capillary; in reality, with hindsight, the needle had entered the vertebral artery with the bevel adhered to the intimate tunic of the vessel. The injection of 2 ml of anesthetic solution, corresponded to the effect of 300 mg of intravenous thiopental. Extracting the syringe, I immediately proceeded to ventilate the patient, who was very easily intubated, without the aid of muscle relaxants; by injecting the 2 ml anesthetic bolus into the vertebral artery, I had also likely anesthetized the cranial nerves. He woke up after 20 minutes, remembering nothing. The surgery was postponed to the next day, under general anesthesia. As always, when these accidents happen, for some time, one is reluctant to repeat a technique that resulted in grave complication. But one day, casually observing a drawing by Buchoj in Winnie’s book in the Italian edition Tecniche Perivascolari di Blocco del Plesso Brachiale [3], I noticed the fascia surrounding the brachial plexus (Figure 1): “Why not cannulate the neuro-vascular bundle along its major axis, then fill it with anesthetic?” This was my first thought. We anesthetists are inclined to cannulate everything.
In this way, the needle was advanced parallel to the upper face of the clavicle and in a non-caudal direction. Therefore, the needle was not directed towards the pleura, avoiding a pneumothorax. Additionally, if the needle had been less than 35-40 mm long, it could not have reached the neuro-vascular structures of the neck. The technique, applied with the paresthesia method, was first published in Minerva Anestesiologica (June 1992) in Italian [4]. In those years the peripheral blocks were based on evocation of paresthesia, “No paresthesias-no anesthesia”, said Daniel C. Moore [2]. After the first publication many other articles were published [7-11]. In 2003, an editorial note appeared at the end of the article, stating that it was the first original Italian technique of loco-regional anesthesia [7]. Middle Interscalene Block (MIB) was the name given to the technique published 14 years later in Regional Anesthesia and Pain Medicine, after having anesthetized, with only the help of an electrostimulator in 719 patients [5]. The aim of MIB is to avoid the most serious complications, which are possible with a supraclavicular caudad approach (pneumothorax) or with a paravertebral technique (subarachnoid or vertebral artery injection); both of which are less frequent nowadays, due to the aid of the electrostimulator and ultrasound guidance utilized concurrently. The name itself (MIB) distinguishes it from the technique of Winnie, which could be defined “High Interscalene Block”.
Patient Position
Upright, seated on the stretcher with the head rest completely raised, with the arm hanging outside the stretcher. Head turned 45° to the opposite side. If it is not possible for the patient to assume this position, the block can also be performed in a supine position, with the arm slightly angled caudally and the head turned 45° to the opposite side.
Landmarks
1) The pulse of the subclavian artery, marked with an O. 2) The midpoint of the clavicle, marked with a dot. 3) The spinous process of C7, marked by an X (Figure 2). A line segment is drawn that goes from the midpoint of the clavicle tangential posterolateral to the O, which marks the pulse of the subclavian artery. We must always have in mind the anatomical arrangement: nerve-artery-vein.
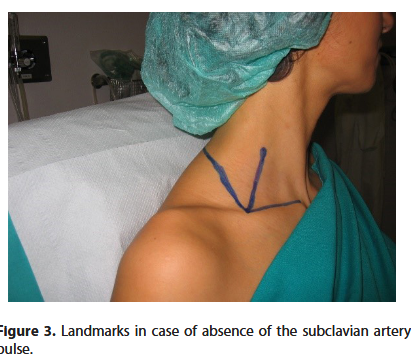
If the subclavian artery pulse is absent, 3 bony landmarks (always present) are used (Figure 3): 1) the midpoint of the clavicle; 2) the spinous process of C7; 3) the sternoclavicular joint.
Connecting the first to the other two we obtain an angle whose bisector corresponds to the brachial plexus. This correlation has been confirmed with an anatomical study [5].
Technique
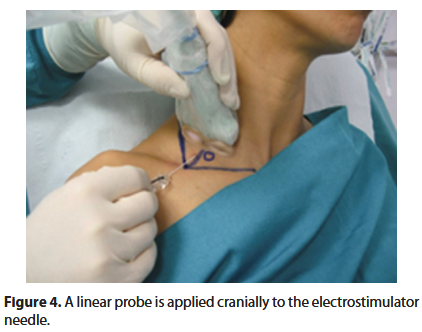
Skin wheal, laterally to the O, (or 1.5-2 cm from the midpoint of the clavicle, on the bisector of the angle) with a 23G needle injecting 2 ml of 1% lidocaine. The 23G needle is replaced by a 35-40 mm, teflon-coated 24G electrostimulator needle. A linear ultrasound probe is applied out of plane cranially to the electrostimulator needle, transversally to the line segment that goes from the midpoint of the clavicle tangential postero-laterally to the O (Figure 4).
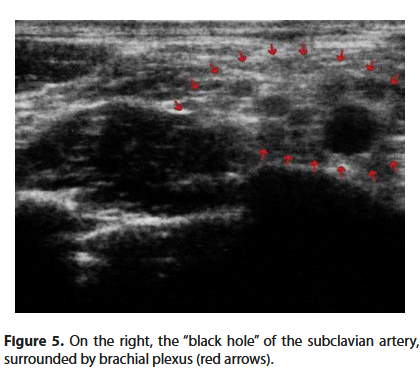
Now we can observe the pulsating black hole of the subclavian artery, surrounded by the transversely cut branches of the brachial plexus (Figure 5).
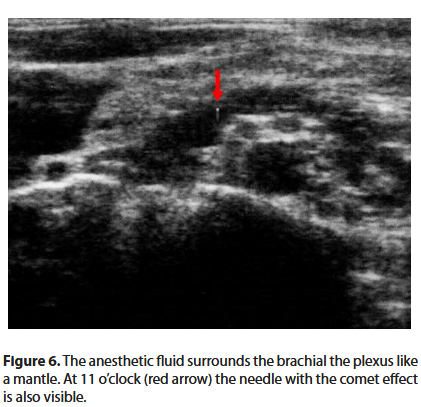
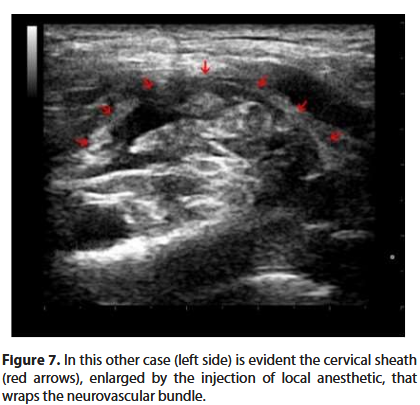
The electrostimulator is set with a current of 0.4 mA. The needle is slowly advanced. When the desired twitch (deltoid, biceps or triceps muscle) appears, the intensity of the current is reduced to below 0.2 mA, until the twitch disappears. In this way we are sure that the tip of the needle is not intraneural. Once the previous stimulation values are restored, 1 ml of anesthetic solution is injected followed by a paraesthesia and the disappearance of the twitch (Raj test) [6]. Only now can we inject the anesthetic solution, witnessing on the screen the expansion of the liquid in the neurovascular bundle (Figures 6 and 7).
Results
The first report of the ultrasound guided middle interscalene block, was described in a poster at the 2008 ESRA Congress in Genoa [12]. Until 2006, with the use of the ENS only, on a population of more than 700 controlled patients, we obtained a success rate of 96.2% [5]. The technique was reported in the book “L’Anestesia Dell’Arto Superiore” in the Italian edition [13], “Anesthesia of the Upper Limb” in the English edition [14] and “Anestesia del Miembro Superior” in the Spanish edition [15]. After having refined the ultrasound guided MIB, we have ascertained that in the period 2013 to 2016, applying the technique to 1,227 patients scheduled for arthroscopic cuff repair, we reached a 100% success rate, without any complication.
Conclusive Considerations
The Middle Interscalene Block may be exclusively attributed to an “out of plain” modality. As a matter of fact, the “in-plane” modality is a difficult procedure, because the concavity of the supraclavicular region poorly suits a linear probe lined up along the plexus direction. However, with the out of plane mode, the poor vision of the needle progression, limited to the tissue’s movements, is counterbalanced by the insertion line’s safety, which has been anatomically demonstrated [5]. The image of local anesthetic spread on ultrasound, injected after ENS, further contributes to controlling the correct position of the needle. In summary, ultrasound application to MIB has allowed an improved safety and success rate to a technique that was previously demonstrated to be safe for the anatomic plane followed by the needle and that, with only the aid of ENS, gave a 96,2% success rate. The echographic implementation has obtained 100% success rate. Therefore, we agree with Admir Hadzic: “…ultrasound and nerve stimulation are complementary and not mutually exclusive monitoring technologies” [16].
Acknowledgments
My thanks to:
Brendan T. Finucane, Professor Emeritus (UAH), Department of Anesthesiology and Pain Medicine University of Alberta, Edmonton, Canada, for having encouraged me in my research, by writing to me: “The information you sent me is very interesting and I intend to incorporate your technique in my future presentations or publications. Like Brown’s method, yours is a very simple concept and appears much safer than the traditional approaches to brachial plexus anaesthesia”.
To the beloved memory of Alon P. Winnie, to whom I sent the book “Anesthesia of the Upper Limb”. He replied: “Having just received the book, I have not finished it, but from what I have read, it is clear it is truly a masterpiece and a wonderful contribution to the understanding of my favourite subject, Brachial Plexus Anesthesia”.
References
2. Moore DC. REGIONAL BLOCK. Springfield, IL: Charles C Thomas Pub Ltd. 1979.
3. Winnie AP. Tecniche Perivascolari di Blocco del Plesso Brachiale. Verduci Editore, Roma 1984.
4. Alemanno F. Un nuovo approccio al plesso brachiale. Minerva Anestesiol. 1992;58:403-406.
5. Alemanno F, Capozzoli G, Egarter-Vigl E, Gottin L, Bartoloni A. The Middle Interscalene Block: Cadaver Study and Clinical Assessment. Regional Anesthesia and Pain Medicine. 2006;31(6):563-568.
6. Ray PP, Rosenblatt R,Montgomery SJ. Use of nerve stimulator for peripheral blocks. Reg Anesth. 1980;5:14-21.
7. Alemanno F, Gretter R, Di Leo Y, Bellini L. Alemanno’s brachial plexus block ten years later topographic study of the anesthetized areas. Minerva Anestesiol. 2003 Jun;69(6): 575-581.
8. Alemanno F, Ghisi D, Fanelli A, Faliva A, Pergolotti B, Bizzarri F, Fanelli G. Tramadol and 0.5% levobupivacaina for single-shot interscalene block: effects on postoperative analgesia in patients undergoing shoulder artroplasty. Minerva Anestesiol. 2012;78(3):291-296.
9. Behr AU, Freo U, Ori C, Westermann B, Alemanno F. Buprenorphine added to levobupivacaine enhances postoperative analgesia of middle Interscalene brachial plexus block. Journal of Anesthesia, 2012;26(5):746-751.
10. Alemanno F, Westermann B, Bettoni A, Candiani A, Cesana BM. Buprenorphine versus Tramadol as perineural adjuvants for postoperative analgesia in patients undergoing shoulder arthroplasty under Middle Interscalene Block. A retrospektive study. Minerva Anestesiologica. 2014;80(11):1198-204.
11. Alemanno F, Ghisi D, Westermann D, Bettoni A, Fanelli A, La Colla L, et al. The use of vitamin B1 as a perineural adjuvant to the Middle Interscalene Block for postoperative analgesia after shoulder surgery. Acta Biomed. 2016;87(1):22-7.
12. Alemanno F. The Ultrasound Guided Middle Interscalene Block. Reg Anesth Pain Med. 2008;33(5):117.
13. Alemanno F, Bosco M, Barbati A. L’ANESTESIA DELL’ARTO SUPERIORE. Roma: Verduci Editore; 2011.
14. Alemanno F, Bosco M, Barbati A. Anesthesia of the Upper Limb – A state of the art guide. Milan, Heidelberg, New York, Dordrecht, London: Springer Verlag; 2014.
15. Alemanno F, Bosco M. Barbati, Anestesia del Miembro Superior. Venezuela, Argentina, Colombia, Guatemala, Mexico, Panamà, Perù: Amolca Editor; 2018.
16. Hadzic A. Nerve Stimulation Should be used in Conjunction with Ultrasound-Guided Nerve Blocks. ASRA NEWS. 2007;7-9.