Keywords
Arteriovenous fistula, Buttonhole technique, Cannulation, Rope-ladder technique, Hemodialysis, MuST
Introduction
One of the most important renal nursing procedures is the cannulation of a vascular access (VA), a procedure that is carried out on every single dialysis treatment. VA cannulation method is still a procedure that reflects local unit practices and the skill of the individual nurse. Despite the impact needling has on VA survival and patient outcome, no universal or standardized method has been proposed for cannulation [1]. Observational data reveals a large variation in how different cannulation techniques are applied in clinical practice. Techniques such as buttonhole (BH), rope ladder (RL), and area cannulation (AC) are often applied in different ways, resulting in different results, which confounds interpretation of the available evidence [2]. For example, in several randomized controlled trials (RCT) [3-5] comparing RL and BH cannulation techniques, researchers described the implementation of BH in some detail but did not define how they implemented RL. What is known is that RL consists of using the entire length of the available vessel through progressive rotation with equal distribution of the cannulation sites at each dialysis session, following a diagram showing the characteristics of each individual arteriovenous fistula (AVF) [6]. BH technique requires different skills from RL, as the AVF needs to be repeatedly cannulated at exactly the same site, using the same insertion angle and the same depth of penetration every time. The available literature does not currently recommend the routine use of BH in all AVF, due to the high risk of infection, but BH may be appropriate for patients with a short cannulation segment [7]. Cannulators using AC also create new puncture sites each time, but with all sites placed in the same area, one rarely larger than 2–3 cm in diameter. The different cannulation techniques (CT) have been investigated, with guidelines stating AC should not be used because of the increased risk of complications such as aneurysms and hemorrhage [8]. VA CT have not seen any development in recent years and in the most recently updated KDOQI [9] guidelines state that rigorous studies assessing cannulation practices to achieve zero complications are necessary. To answer this challenge, a new approach to fistula cannulation with apparent benefits for patients has been used since 2013, the Multiple Single cannulation Technique (MuST) [6,10].
With this comment, we intend to discuss and present other results that emerged from the implementation of the MuST project.
How to Implement MuST
How can nurses reduce AC, without a more widespread use of BH? This was the starting point for the MuST project. MuST was implement via a pilot project in a single dialysis clinic known for a good vascular access management, and a few patients were enrolled. MuST gained immediate patient acceptance for two main reasons: reduction of pain associated with cannulations and reduction in the infiltration rate. MuST also gained immediate nursing team acceptance due to the ease of implementation of this new CT. The success of this pilot project led to the decision to implement the MuST project [6] across the entire NephroCare Portugal dialysis network. After MuST project gained approval by the ethics committee, the multidisciplinary team was trained in the goals of this CT and the rules for implementing the project. Successful project implementation required the involvement of the head nurse, medical director, and VA coordinator of each dialysis unit. The role played by the head nurse in promoting the project and conducting regular meetings with the team was crucial.
The project was three-fold:
- Continuous support from the head nurse and clinical director, team motivation, and confidence in the new CT;
- Patient involvement in fistula self-care;
- Regular team meetings and discussion of each participant selected, results sharing, and the follow-up of all selected patients.
The MuST CT was recently described in detail [10], and the MuST study [6] presents the first comparison of MuST with BH and RL.
Since 2013, the majority of data have shown that MuST is safe, can be trusted, and above all is useful for patients, allowing AVF survival comparable to the results obtained with RL [6]. However, more studies are needed to consolidate these findings. The experience with MuST over the past seven years has been in both new AVFs and AVs previously cannulated with other CTs. It has been used in distal and proximal AVF with good results. Plastic cannulas are used in patients with metal allergies, which means MuST can be used with no limitations or changes in dialytic outcomes. A descriptive study [11] found good treatment outcomes when using plastic cannulas, Kt/ V=1.87 SD=0.25 and substitution volume 23.9L SD=4.56.
MuST in New AVFs
Cannulation is an essential skill for dialysis nurses. The failure to correctly repeat this procedure safely and effectively may result in serious complications for the patient, making any new AVF cannulation stressful for health care professionals (HCP). A cross-sectional survey [12] conducted in 171 dialysis units located in Europe, the Middle East and Africa reported that in 10,807 cannulation procedures evaluated in the same number of patients, the need for multiple-cannulation (33.8%) was the most frequent complication. The correct choice of cannulation technique is a factor that can contribute to procedure success and patient safety; an inadequate and unsuccessful choice increases the risk of AVF loss. A RCT [13] comparing BH with RL, showed lack of survival benefit and higher risk of AVF infection, when promoting buttonhole needling. The use of MuST in new fistulas is easy to identify the cannulation sites, thus dispensing the need to use a diagram. The identification of sites through pigmentation changes usually occurs after 8 to 12 consecutive cannulations. In previously used fistulas, this identification occurs much later and varies from patient to patient. Was also evaluated the presence of and scab size at the cannulation sites and found no difference between new or previously used fistulas.
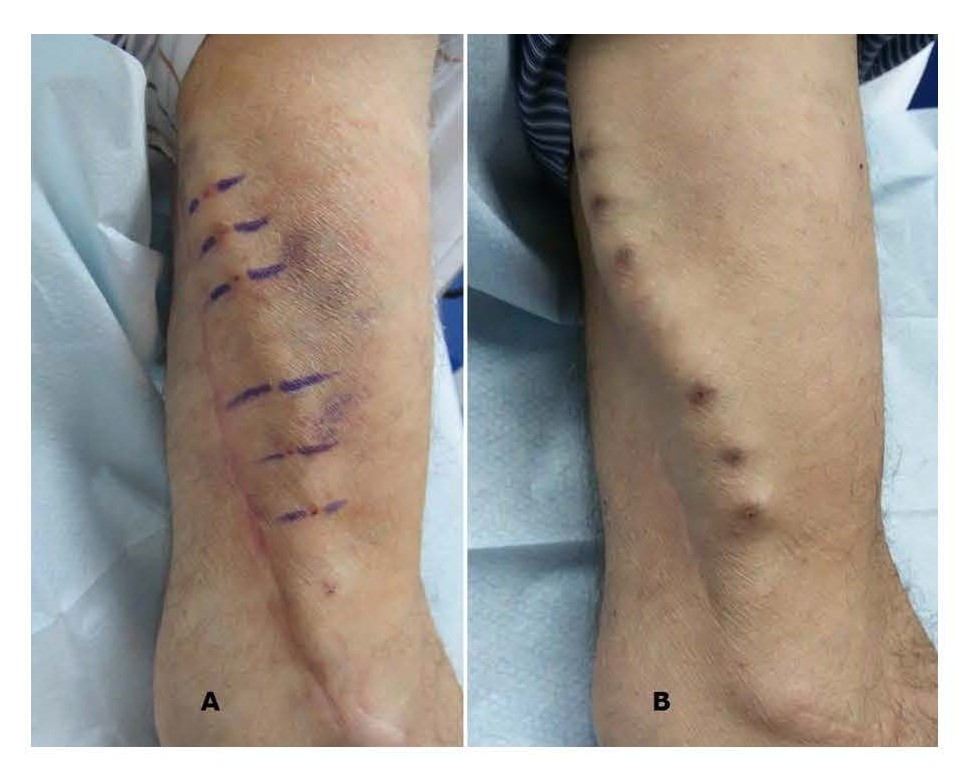
One possible limitation from MuST implementation is perhaps the slight difficulty experienced in identifying the cannulation sites at an early stage, even with the use of a skin pencil (Figure 1).
Figure 1. A. Skin pencil marking of cannulation sites at the beginning of MuST. The cannulation sites are exactly in the center of the line. B. Arteriovenous fistula in the same patient after 2 years of use. Cannulation sites are easily identifiable.
The most common complication of MuST cannulation was needle infiltration or hematoma, as reported by Sousa et al. [14]. The rate of hematoma in MuST was 2.29 per 1000 dialysis sessions, results which are much lower than those presented by MacRae et al. [4] who, in a randomized control trial, enrolling 140 patients, reported fewer hematomas with BH (295/1000 dialysis sessions with BH versus 436/1000 dialysis sessions with standard cannulation).
According to Ibeas et al. [15], repeated venous cannulation alone can lead to AVF damage due to direct microtrauma from the puncture and/or increased endothelial damage caused by shear forces created during blood return. However, in the MuST study [6], MuST was seen to preserve the AVF pathway, with only one patient developing an aneurysm.
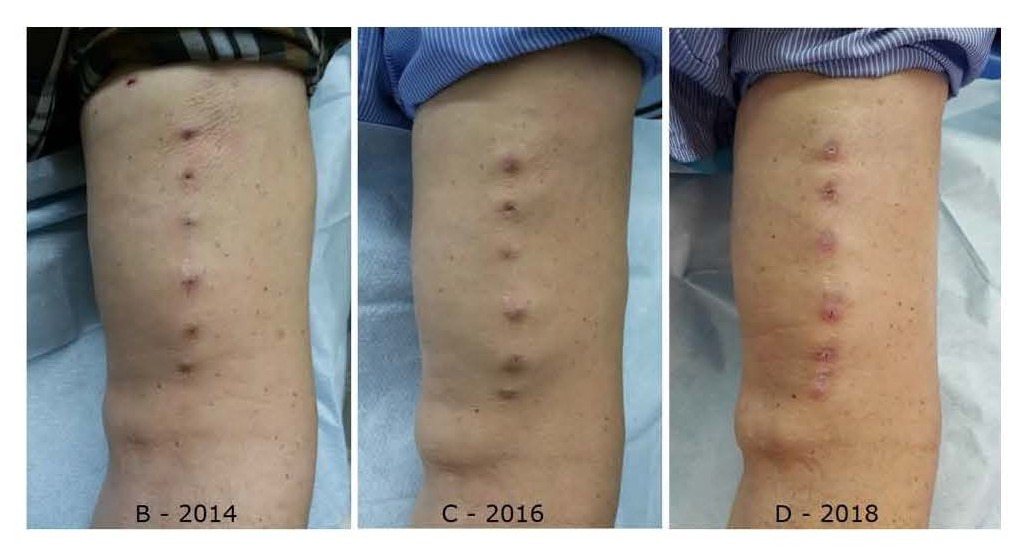
An observation of MuST use in a patient over the course of 5 years shows that the new AVF, remains the same diameter throughout the venous segment, irrespective of AVF location, as Figure 2 shows.
Figure 2. MuST evolution in a new left brachial cephalic arteriovenous fistula in the same patient. After 6 years of using the same spots, there was no aneurysmal development, despite being a proximal fistula with blood flow > 2000 mL measured by thermodilution. A. the start of cannulation in 2013; D. 2018.
MuST in Previously Used AVF
Using MuST on previously used AVFs which had already been cannulated using other techniques such as AC and BH appears to be safe and reliable and in addition that it is possible to adapt CT to each vascular access segment.
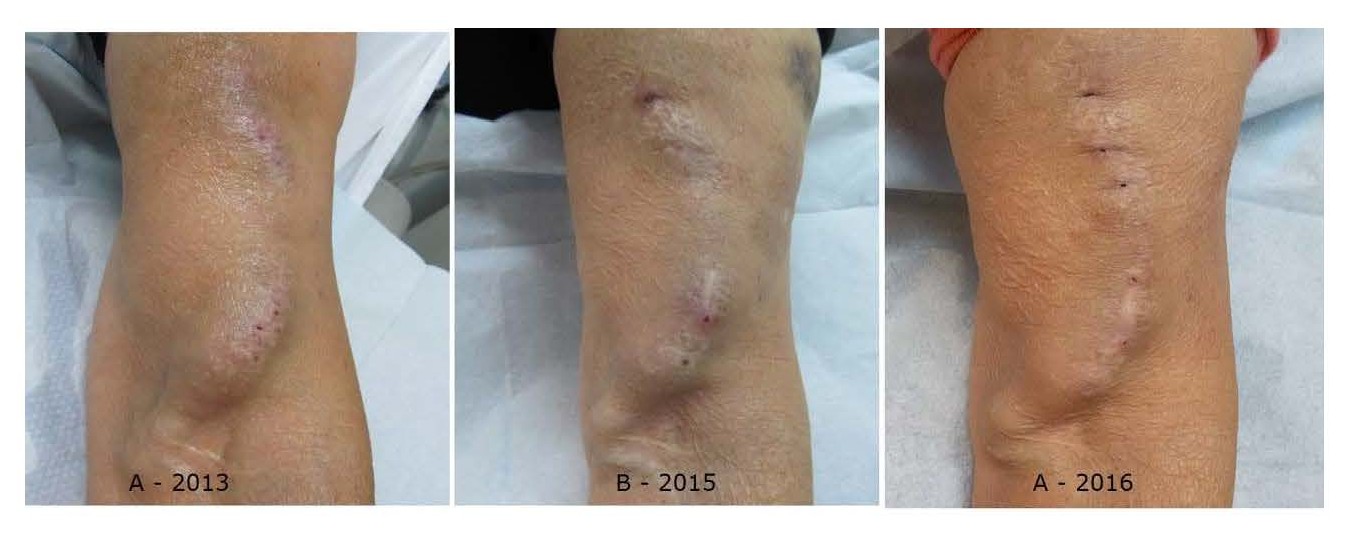
Figure 3 shows the switch of CT in a patient’s vascular access over a course of 3 years. Here, an aneurism reduction was observed after initiating BH, but pain experienced by the patient during cannulation, and difficulties in scab removal, made a change to MuST necessary. Although the nursing team has been deeply involved with this procedure, this is a very demanding process, as it needs more attention by nurses, evaluating the application of MuST mainly in AVF with aneurysms.
Figure 3. 3 images of the same patient, who was previously cannulated, with aneurysm development in the arterial cannulation area. From 2013 – 2015 he underwent buttonhole cannulation and was then switched to MuST (A- 2016 after one year).
MuST Compared to Buttonhole
Studies have reported a significant increased risk of both systemic or localized infections for BH compared to standard needling [3]. In an RCT [13], 70 patients in BH were recruited, 12 developed an infection during study follow-up.
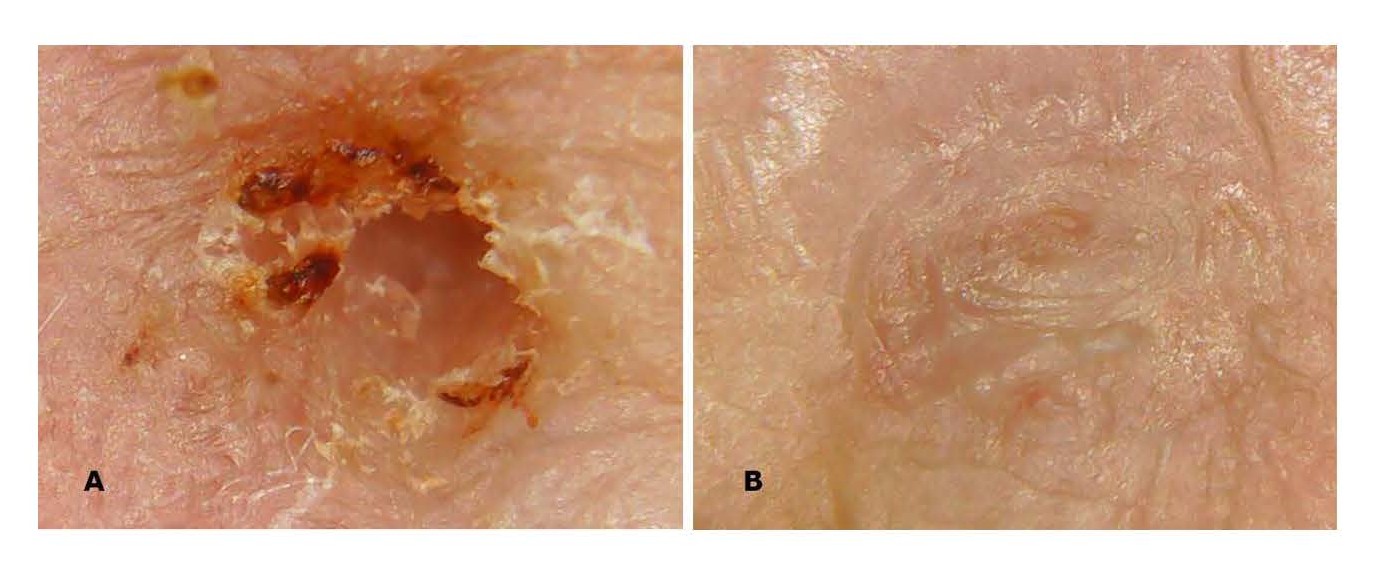
This increased risk is usually related to failures in the disinfection protocol, and scab problems. O’Brien et al. [16] state that the cannulation site becomes similar to a chronic ulcer and, despite disinfection methods, it is possible that the overlying skin colonizers remain at the time of cannulation. However, one major advantage of MuST is good healing of the cannulation spots, which minimizes scab problems.
When comparing the size of cannulation spot scabs, Sousa et al. [17] showed that the scab size is smaller in patients in whom MuST is performed (mean scab size of MuST 4.01 mm2versus BH 10.32 mm2, t=7.075, p<0.001), and 20% of the patients had no evidence of scab at all. If a scab is present, it is normally easily removed during disinfection and the cannulation spot always heals (Figure 4). There is no need to use any other technique to remove the scabs. Picture A of Figure 4 shows that with the BH, even once the scab is removed, small particles remain from the healing process that are not removed with disinfection and that are later introduced into the patient`s circulation, increasing the risk of bacteremia.
Figure 4. A. Buttonhole tunnel after scab removal. B. Fibrotic spot in MuST after scab removal. Picture captured with USB digital microscope 500X.
Moreira et al. [18] reported two cases of significant stenosis associated with BH and an associated risk of thrombosis. Our experience also showed some cases of stenotic development of the vein segment not punctured, in which the switch to MuST promoted the vein dilation to normal diameter (Figure 5).
Figure 5. A: Stenosis associated with BH cannulation. B: Vessel segment normal diameter again after MuST was started.
Patients’ and HCPs’ perceptions of MuST CT were sought, in answers to a dialysis unit questionnaire, most of the nurses (95%) stated that MuST is the CT with the most advantages for patients and professionals [19].
Acknowledging that fistula cannulation is a procedure which requires skill, nurses admitted to using their preferred form of CT, a factor which can impact on the decision choice. But they say that the decision is made by a multidisciplinary team with the goal of selecting the best CT for all vascular access. Patients’ opinion on CT was that the most common advantages of MuST were less pain and less hematomas than with BH.
The other advantage observed since the implementation of MuST has been the use of standard sharp dialysis needles, which offers advantages over BH such as cost reduction, fewer complications in the cannulation process, easier application and increased HCP satisfaction.
MuST Compared to Rope Ladder
In a meta-analysis [20], comparing RL with BH, it was not concluded which CT has been associated to better AVF survival outcomes. However, as already described in MuST study, similar survival curves are observed in both RL and MuST, indicating that MuST is as similarly safe to use as RL [6] and both showed better results compared to BH .
Despite its proven safety, RL is not without its drawbacks. Parisotto MT et al. [12] identified that unsuccessful cannulation of RL was related to pain and fear of missed cannulations, which can lead to patients abandoning this CT. In MuST study, no patients abandoned MuST for reasons related to pain or other factors, although 4 patients abandoned RL due to pain during the cannulation moment. Pain and discomfort perceived by patients caused by VA cannulation are of major concern for dialysis patients.
One major success factor for a proper RL implementation is a VA diagram showing the site of the last cannulation and where following cannulations should be performed. In the presence of multiple scabs and without this aid, identifying where to cannulate is difficult if not impossible, leading to an easier way being taken: to cannulate in a more obvious location, leading to AC. Using MuST, in which the cannulation sites are easily identifiable, this situation is also greatly minimized.
Harwood et al. [21] identified that a successful AVF cannulation was also connected to listening to patients’ fears in regard to the pain and anxiety that can occur in cannulation. An aim of this group was to find a way of performing successful cannulations with good acceptance from patients and nurses. It was observed that MuST was well accepted by patients (less pain, fewer cannulation incidents), and by the nursing team.
Conclusion
While BH is associated with an increase in infections [3-5] and is complex to perform [22-24], leading to its abandonment, a lack of an orientation diagram to aid in performing RL leads the cannulator to inevitably use the area CT [25] or invariably to technique abandonment, with the pain of cannulation being a factor to consider here.
The results of MuST [6] suggest that while the use of MuST cannulation in hemodialysis patients is efficacious, safe, and with a survival rate identical to RL, further studies are needed to demonstrate its benefits and advantages.
Abbreviations
MuST: Multiple Single Cannulation Technique; VA: Vascular Access; BH: Buttonhole; RL: Rope Ladder; AC: Area Cannulation; RCT: Randomized Controlled Trials; AVF: Arteriovenous Fistula; CT: Cannulation Techniques; HCP: Health Care Professionals
Financial Disclosure
The authors declare no funding was received for this study.
Conflicts of Interest
The authors declare no relevant conflicts of interest.
References
2. Gallieni M, Hollenbeck M, Inston N, Kumwenda M, Powell S, Tordoir J, et al. Clinical practice guideline on peri-and postoperative care of arteriovenous fistulas and grafts for haemodialysis in adults. Nephrology Dialysis Transplantation. 2019 Jun 1;34(Supplement_2):ii1-42.
3. Chow J, Rayment G, Miguel SS, Gilbert M. A randomised controlled trial of buttonhole cannulation for the prevention of fistula access complications. Journal of Renal Care. 2011 Jun;37(2):85-93.
4. MacRae JM, Ahmed SB, Atkar R, Hemmelgarn BR. A randomized trial comparing buttonhole with rope ladder needling in conventional hemodialysis patients. Clinical Journal of the American Society of Nephrology. 2012 Oct 1;7(10):1632-8.
5. MacRae JM, Ahmed SB, Hemmelgarn BR, Alberta Kidney Disease Network. Arteriovenous fistula survival and needling technique: long-term results from a randomized buttonhole trial. American Journal of Kidney Diseases. 2014 Apr 1;63(4):636-42.
6. Peralta R, Fazendeiro Matos J, Pinto B, Gonçalves P, Sousa R, Felix C, et al. Multiple single cannulation technique of arteriovenous fistula: A randomized controlled trial. Hemodialysis International. 2021 Jul 6.
7. Schmidli J, Widmer MK, Basile C, de Donato G, Gallieni M, Gibbons CP et al. Editor's choice–vascular access: 2018 clinical practice guidelines of the European Society for Vascular Surgery (ESVS). European Journal of Vascular and Endovascular Surgery. 2018 Jun 1;55(6):757-818.
8. Staaf K, Fernström A, Uhlin F. Cannulation technique and complications in arteriovenous fistulas: a Swedish Renal Registry-based cohort study. BMC Nephrology. 2021 Dec;22(1):1-2.
9. Lok CE, Huber TS, Lee T, Shenoy S, Yevzlin AS, Abreo K, et al. KDOQI clinical practice guideline for vascular access: 2019 update. American Journal of Kidney Diseases. 2020 Apr 1;75(4):S1-64.
10. Peralta R. Safe Needling of Arteriovenous Fistulae in Patients on Hemodialysis: Literature Review and a New Approach. Nephrology Nursing Journal. 2021 Mar 1;48(2).
11. Sousa R, Silva A, Coimbra M, Gonçalves P, Matos JF. Patients and nurses perspectives about plastic cannulae for arteriovenous fistula. In: [Abstract] EDTNA/ERA Abstract Book. 2019. p. 55.
12. Parisotto MT, Pelliccia F, Grassmann A, Marcelli D. Elements of dialysis nursing practice associated with successful cannulation: result of an international survey. The Journal of Vascular Access. 2017 Mar;18(2):114-9.
13. MacRae JM, Ahmed SB, Hemmelgarn BR, Alberta Kidney Disease Network. Arteriovenous fistula survival and needling technique: long-term results from a randomized buttonhole trial. American Journal of Kidney Diseases. 2014 Apr 1;63(4):636-42.
14. Sousa R, Silva A, Coimbra M, Gonçalves P, Peralta R, Matos JF. Multiple single puncture cannulation technique – 5-year results. [Abstract] EDTNA/ERA Abstr B. 2018;60.
15. Ibeas J, Roca-Tey R, Vallespín J, Moreno T, Moñux G, Martí-Monrós A, et al. Guía Clínica española del acceso vascular para hemodiálisis. Nefrología. 2017 Nov 1;37:1- 91.
16. O'Brien FJ, Kok HK, O'Kane C, McWilliams J, O'Kelly P, Collins P, et al . Arterio-venous fistula buttonhole cannulation technique: a retrospective analysis of infectious complications. Nephrology Dialysis Transplantation Plus. 2012 Dec 1;5(6):526-9.
17. Sousa R, Silva A, Coimbra M, Gonçalves P, Matos JF. Must cannulation technique minimizes cannulation site problems. [Abstract] EDTNA/ERA Abstr B. 2019;66.
18. Moreira CL, Castro A, Silva F, Almeida P, de Matos AN, Sousa CN, et al. Stenosis and thrombosis—unveiled complications of buttonhole cannulation. Hemodialysis International. 2019 Jul;23(3):E90-2.
19. Ren C, Han X, Huang B, Yuan L, Cao Y, Yang X. Efficacy of buttonhole cannulation (BH) in hemodialysis patients with arteriovenous fistula: a meta-analysis. International Journal of Clinical and Experimental Medicine. 2016 Jan 1;9(8):15363-70.
20. Harwood LE, Wilson BM, Oudshoorn A. Improving vascular access outcomes: attributes of arteriovenous fistula cannulation success. Clinical Kidney Journal. 2016 Apr 1;9(2):303-9.
21. van Loon MM, Goovaerts T, Kessels AG, van der Sande FM, Tordoir JH. Buttonhole needling of haemodialysis arteriovenous fistulae results in less complications and interventions compared to the rope-ladder technique. Nephrology Dialysis Transplantation. 2010 Jan 1;25(1):225-30.
22. Dinwiddie LC, Ball L, Brouwer D, Doss-McQuitty S, Holland J. What nephrologists need to know about vascular access cannulation. Seminars in Dialysis. 2013 May;26(3):315-322.
23. Smyth W, Hartig V, Manickam V. Outcomes of buttonhole and rope-ladder cannulation techniques in a tropical renal service. Journal of Renal Care. 2013 Sep;39(3):157-65.
24. Stolic RV, Trajkovic GZ, Kostic MM, Lazic BD, Odalovic B, Smilic TN, et al. Cannulation Technique and Arteriovenous Fistula Survival in Older Adult Patients on Hemodialysis. Nephrology Nursing Journal. 2017 Sep 1;44(5).